The left ventricular ejection fraction (LVEF) is a crucial measure of heart function, indicating the percentage of blood pumped out of the left ventricle with each heartbeat. A normal LVEF ranges between 55% and 70%. When the LVEF falls below this range, it signals a potential issue with the heart’s ability to pump blood effectively. In this comprehensive guide, we delve into the various causes of low left ventricular ejection fraction, exploring the underlying conditions, risk factors, diagnostic methods, and treatment options associated with this critical cardiac parameter.
Understanding Left Ventricular Ejection Fraction
Before delving into the causes of low LVEF, it’s essential to understand how this parameter is measured and its significance in assessing heart function. The left ventricle is responsible for pumping oxygen-rich blood to the body. During each heartbeat, a certain amount of blood is ejected from the left ventricle into the aorta, which then delivers it to the rest of the body.
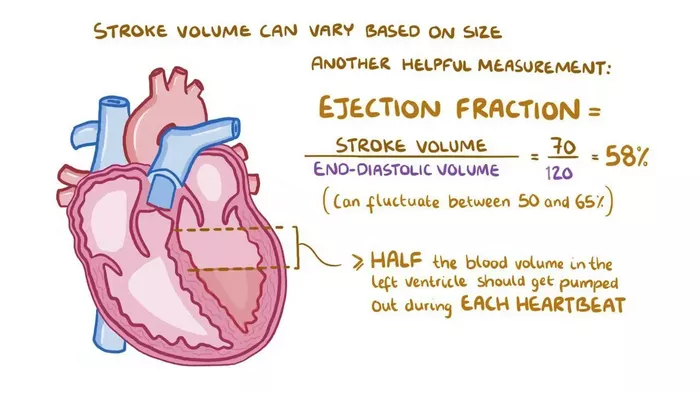
The LVEF is expressed as a percentage and is calculated by dividing the volume of blood ejected from the left ventricle during systole (the contraction phase of the heart cycle) by the total volume of blood in the left ventricle at the end of diastole (the relaxation phase). This measurement provides valuable information about the heart’s efficiency in pumping blood and is a key parameter in diagnosing and managing various cardiac conditions.
Causes of Low Left Ventricular Ejection Fraction
1. Coronary Artery Disease (CAD): One of the primary causes of low LVEF is coronary artery disease, a condition characterized by the narrowing or blockage of coronary arteries that supply blood to the heart muscle. Reduced blood flow to the heart can lead to myocardial ischemia (lack of oxygen to the heart muscle), which in turn impairs the heart’s pumping ability and lowers the LVEF.
2. Myocardial Infarction (Heart Attack): A myocardial infarction, commonly known as a heart attack, occurs when a coronary artery becomes blocked, cutting off blood supply to a part of the heart muscle. The resulting damage to the heart tissue can significantly reduce the LVEF, especially if the infarction affects a large area of the left ventricle.
3. Cardiomyopathy: Cardiomyopathy refers to diseases of the heart muscle that can weaken the heart and impair its pumping function. Dilated cardiomyopathy, in which the heart chambers become enlarged and weakened, is often associated with a low LVEF due to decreased contractility of the left ventricle.
4. Valvular Heart Disease: Certain heart valve disorders, such as aortic stenosis (narrowing of the aortic valve) or mitral regurgitation (leakage of the mitral valve), can lead to increased pressure in the left ventricle, causing it to work harder to pump blood. Over time, this can result in a decreased LVEF.
5. Hypertension (High Blood Pressure): Chronic high blood pressure can strain the heart muscle, leading to left ventricular hypertrophy (thickening of the left ventricle walls) and eventual impairment of ventricular function. This can contribute to a lower LVEF.
6. Heart Failure: Heart failure is a condition in which the heart is unable to pump enough blood to meet the body’s needs. Both systolic heart failure (reduced ability of the heart to contract and pump blood) and diastolic heart failure (impaired relaxation and filling of the heart chambers) can result in a decreased LVEF.
7. Arrhythmias: Abnormal heart rhythms, such as atrial fibrillation or ventricular tachycardia, can affect the coordination of heart contractions and reduce the efficiency of blood ejection from the left ventricle, leading to a lower LVEF.
8. Infections and Inflammation: Conditions such as myocarditis (inflammation of the heart muscle) or endocarditis (infection of the heart valves) can directly damage heart tissue and impair ventricular function, contributing to a decrease in LVEF.
9. Toxic Effects: Exposure to certain toxins, such as alcohol or certain chemotherapy drugs, can damage heart cells and interfere with cardiac function, leading to a reduced LVEF.
Diagnostic Evaluation
Diagnosing low LVEF typically involves a comprehensive evaluation that may include:
1. Echocardiography: A non-invasive imaging technique used to assess heart structure and function, including LVEF measurement.
2. Cardiac MRI or CT scan: These imaging studies can provide detailed information about heart anatomy, function, and tissue characteristics.
3. Blood tests: Biomarkers such as B-type natriuretic peptide (BNP) or N-terminal pro-B-type natriuretic peptide (NT-proBNP) may be elevated in heart failure and other cardiac conditions.
4. Coronary angiography: An invasive procedure to visualize the coronary arteries and assess for blockages or narrowing.
Electrophysiological studies: These tests evaluate heart rhythm abnormalities and their impact on cardiac function.
Treatment Approaches
The management of low LVEF depends on the underlying cause and may involve:
1. Lifestyle modifications: Including a heart-healthy diet, regular exercise, smoking cessation, and stress management.
2. Medications: Such as ACE inhibitors, beta-blockers, diuretics, and anti-arrhythmic drugs to control blood pressure, improve heart function, and manage arrhythmias.
3. Revascularization procedures: Like coronary artery bypass grafting (CABG) or percutaneous coronary intervention (PCI) to restore blood flow to the heart in cases of coronary artery disease.
4. Valve repair or replacement: For patients with significant valvular heart disease.
5. Implantable devices: Such as pacemakers, implantable cardioverter-defibrillators (ICDs), or cardiac resynchronization therapy (CRT) devices to regulate heart rhythm and improve pumping efficiency.
6. Surgical interventions: In some cases, surgical procedures like ventricular assist device (VAD) implantation or heart transplantation may be necessary for advanced heart failure.
Conclusion
Low left ventricular ejection fraction is a critical marker of cardiac function that can result from a wide range of underlying conditions, including coronary artery disease, myocardial infarction, cardiomyopathy, valvular heart disease, hypertension, and arrhythmias, among others. Early detection, accurate diagnosis, and tailored treatment strategies are essential in managing this condition and improving patient outcomes. Collaborative efforts between healthcare providers, including cardiologists, cardiac surgeons, and allied health professionals, play a key role in delivering comprehensive care to individuals with low LVEF.