Hypertension, commonly known as high blood pressure, is a significant risk factor for the development of atherosclerosis, a condition characterized by the buildup of plaque in the arteries. This article delves into the intricate relationship between hypertension and atherosclerosis, exploring the mechanisms through which hypertension contributes to the progression of this cardiovascular disease.
Understanding Hypertension
To grasp the connection between hypertension and atherosclerosis, it’s essential to first understand what hypertension entails. Blood pressure is the force exerted by circulating blood against the walls of blood vessels. When this pressure remains consistently elevated over time, it leads to hypertension. This condition is often asymptomatic but can have serious implications for cardiovascular health if left uncontrolled.
The Role of Atherosclerosis
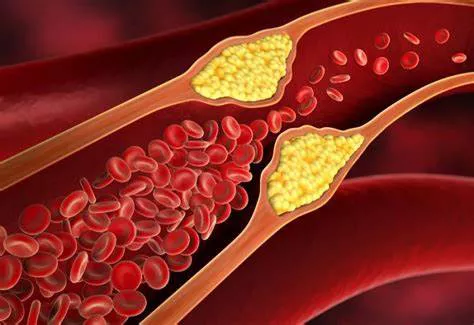
Atherosclerosis is a progressive condition characterized by the accumulation of cholesterol, fatty substances, cellular waste products, and calcium deposits in the inner lining of arteries. This buildup forms plaques that can narrow and stiffen arteries, reducing blood flow to vital organs such as the heart, brain, and kidneys. Atherosclerosis is a major contributor to cardiovascular diseases like coronary artery disease, stroke, and peripheral artery disease.
Impact of Hypertension on Arterial Health
Hypertension exerts several direct and indirect effects on arterial health, contributing to the development and progression of atherosclerosis:
1. Endothelial Dysfunction: The inner lining of blood vessels, known as the endothelium, plays a crucial role in maintaining vascular health. High blood pressure can damage endothelial cells, leading to endothelial dysfunction. This dysfunction disrupts the balance of vasoconstrictive and vasodilatory substances, promoting inflammation and the accumulation of plaque.
2. Increased Oxidative Stress: Hypertension is associated with increased oxidative stress, an imbalance between the production of reactive oxygen species (ROS) and antioxidant defenses. Oxidative stress contributes to endothelial damage, lipid peroxidation, and the initiation of inflammatory pathways that fuel atherosclerosis progression.
3. Inflammatory Response: Chronic hypertension triggers an inflammatory response within arterial walls. Inflammatory cells, such as macrophages and T lymphocytes, infiltrate the vessel walls in response to endothelial injury and lipid deposition. This inflammation further accelerates plaque formation and destabilization.
4. Smooth Muscle Cell Proliferation: Hypertension stimulates the proliferation of smooth muscle cells in arterial walls. These cells contribute to the formation of a fibrous cap over atherosclerotic plaques. However, this cap can become unstable due to ongoing inflammation and mechanical stress, increasing the risk of plaque rupture and thrombosis.
Synergistic Effects of Hypertension and Dyslipidemia
While hypertension and atherosclerosis are distinct entities, they often coexist and interact synergistically to exacerbate cardiovascular risk:
1. Dyslipidemia: Elevated levels of LDL cholesterol (low-density lipoprotein) and reduced levels of HDL cholesterol (high-density lipoprotein) are common features of atherosclerosis. Hypertension can exacerbate dyslipidemia by promoting LDL oxidation, impairing HDL functionality, and altering lipid metabolism in ways that favor plaque formation and progression.
2. Endothelial Injury: Both hypertension and dyslipidemia contribute to endothelial injury, creating a vicious cycle of inflammation, oxidative stress, and plaque development. The combination of high blood pressure and dyslipidemia significantly increases the likelihood of atherosclerotic complications such as myocardial infarction and stroke.
Clinical Implications and Management Strategies
Given the intricate interplay between hypertension and atherosclerosis, effective management strategies should target both conditions comprehensively:
1. Blood Pressure Control: Tight control of blood pressure is paramount in reducing the risk of atherosclerosis-related events. Lifestyle modifications, including dietary changes, regular exercise, weight management, and stress reduction, are fundamental aspects of blood pressure management. Pharmacological interventions, such as antihypertensive medications, may also be necessary depending on individual risk profiles.
2. Lipid Management: Addressing dyslipidemia is essential in mitigating atherosclerosis progression. This involves dietary modifications, increased physical activity, smoking cessation, and, when indicated, lipid-lowering medications such as statins or fibrates. Achieving optimal lipid levels can help stabilize plaques and reduce the risk of cardiovascular events.
3. Antiplatelet Therapy: In certain high-risk individuals, antiplatelet agents like aspirin may be prescribed to reduce the risk of thrombotic events associated with unstable atherosclerotic plaques. However, the decision to initiate antiplatelet therapy should be individualized based on a thorough assessment of cardiovascular risk factors and bleeding risk.
4. Lifestyle Modification: Encouraging lifestyle changes is integral to long-term cardiovascular health. This includes promoting a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins, limiting sodium and saturated fat intake, moderating alcohol consumption, avoiding tobacco use, and engaging in regular physical activity.
Conclusion
Hypertension and atherosclerosis are intertwined in a complex web of pathophysiological mechanisms that contribute to cardiovascular morbidity and mortality. Understanding the link between these conditions is crucial for implementing effective preventive and therapeutic strategies. By addressing hypertension, managing dyslipidemia, and promoting a healthy lifestyle, individuals can reduce their risk of atherosclerosis-related complications and improve overall cardiovascular outcomes.