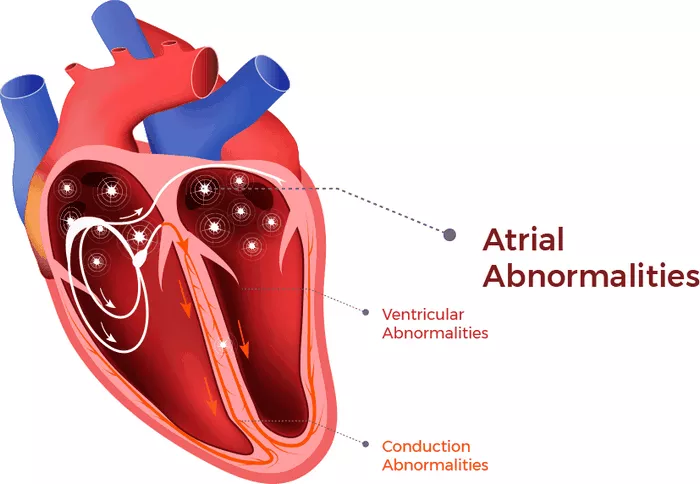
Atrial Fibrillation (Afib) is a common cardiac arrhythmia characterized by rapid and irregular electrical activity in the atria of the heart. It affects millions of people worldwide and is associated with an increased risk of stroke. Understanding why Afib leads to stroke is crucial for healthcare professionals, patients, and researchers alike. This article delves into the mechanisms underlying this relationship and explores the preventive strategies and treatments available.
The Link Between Afib and Stroke
Thrombus Formation
One of the primary mechanisms by which Afib leads to stroke is through the formation of blood clots or thrombi. In Afib, the irregular and rapid contractions of the atria disrupt normal blood flow, leading to stasis or pooling of blood in the atria. This stagnant blood is more prone to clot formation, particularly in the left atrial appendage (LAA), a small pouch in the left atrium known for its propensity to harbor clots.
When a clot forms in the LAA, it can dislodge and travel through the bloodstream. If it reaches the brain’s blood vessels, it can block a vessel (cerebral artery) and prevent oxygenated blood from reaching parts of the brain. This blockage, known as an ischemic stroke, can result in brain tissue damage and neurological deficits.
Embolic Events
The term “embolism” refers to the obstruction of a blood vessel by an embolus, which is usually a blood clot or other foreign material. In Afib, embolic events can occur when a clot formed in the atria dislodges and travels to other organs besides the brain. This can lead to complications such as mesenteric ischemia (inadequate blood supply to the intestines), renal infarction (damage to the kidney due to lack of blood flow), or limb ischemia (restricted blood flow to the extremities).
While strokes are the most concerning embolic events associated with Afib due to their potential for significant morbidity and mortality, it’s essential to recognize that other organs can also be affected by emboli originating from the heart.
Risk Factors for Stroke in Afib Patients
Increased Age
Age is a significant risk factor for both Afib and stroke. As individuals age, the prevalence of Afib rises, as does the risk of stroke. This is partly due to age-related changes in the heart’s structure and function, as well as the cumulative effect of other risk factors over time.
Hypertension (High Blood Pressure)
Hypertension is a well-established risk factor for stroke in general, and it also contributes significantly to the risk of stroke in Afib patients. Elevated blood pressure can damage blood vessels, including those in the brain, making them more susceptible to the effects of clot formation or embolism.
Diabetes Mellitus
Diabetes is associated with an increased risk of cardiovascular disease, including Afib and stroke. High blood sugar levels can lead to vascular changes that promote clot formation and atherosclerosis (hardening and narrowing of arteries), further raising the risk of stroke in individuals with Afib.
Heart Failure
Heart failure, especially if it involves reduced ejection fraction (a measure of the heart’s pumping ability), is a significant risk factor for stroke in Afib patients. The combination of impaired heart function, blood stasis, and potential clot formation in the atria significantly elevates the risk of embolic events, including stroke.
Previous Stroke or Transient Ischemic Attack (TIA)
Individuals who have experienced a prior stroke or TIA are at increased risk of subsequent strokes, particularly if they have Afib. The presence of Afib amplifies the risk of recurrent strokes due to the ongoing potential for embolic events from the heart.
Preventive Strategies and Treatment
Anticoagulation Therapy
Anticoagulants, commonly referred to as blood thinners, are a cornerstone of stroke prevention in Afib patients. These medications work by inhibiting the clotting cascade, reducing the formation of blood clots and the risk of embolic events. Warfarin and newer direct oral anticoagulants (DOACs) such as dabigatran, rivaroxaban, apixaban, and edoxaban are widely used for this purpose.
The choice of anticoagulant and dosing regimen depends on various factors, including the patient’s age, renal function, risk of bleeding, and potential drug interactions. Regular monitoring and dose adjustments are often necessary to ensure optimal efficacy and safety.
Rate and Rhythm Control
Managing the heart rate and rhythm in Afib patients is another key aspect of treatment. Rate control aims to keep the heart rate within a target range to reduce symptoms and prevent tachycardia-related complications. Rhythm control strategies, such as antiarrhythmic medications or procedures like catheter ablation, aim to restore and maintain normal sinus rhythm to alleviate symptoms and potentially reduce the risk of thrombus formation.
Left Atrial Appendage Closure (LAAC)
Given the role of the LAA in thrombus formation in Afib, closing off this structure can be an effective strategy for stroke prevention, particularly in patients who are unable to take anticoagulant medications or have a high bleeding risk. LAAC can be achieved through surgical ligation or less invasive techniques such as percutaneous occlusion devices.
Lifestyle Modifications
Encouraging lifestyle modifications is essential in managing Afib and reducing stroke risk. This includes maintaining a healthy weight, regular physical activity, a balanced diet low in sodium and saturated fats, smoking cessation, moderation of alcohol consumption, and effective management of comorbid conditions such as hypertension, diabetes, and hyperlipidemia.
Conclusion
Atrial Fibrillation significantly increases the risk of stroke through mechanisms such as thrombus formation and embolic events originating from the heart. Understanding the interplay between Afib and stroke risk factors is crucial for effective prevention and management strategies. Anticoagulation therapy, rate, and rhythm control measures, left atrial appendage closure, and lifestyle modifications are key components of comprehensive care for Afib patients aimed at reducing the incidence and impact of stroke. Healthcare professionals play a pivotal role in educating patients about their condition, optimizing treatment strategies, and monitoring for potential complications to improve outcomes and quality of life.