The Mechanisms Behind Sepsis-Induced Hypotension
Sepsis is a life-threatening condition that occurs when the body’s response to an infection triggers widespread inflammation, leading to organ dysfunction. One of the hallmark signs of sepsis is hypotension, a dangerous drop in blood pressure that can significantly impact a patient’s prognosis. In this article, we will delve into the intricate mechanisms that underlie why sepsis causes hypotension, exploring the role of inflammation, vasodilation, cardiovascular dysfunction, and other factors.
Understanding Sepsis and Its Impact on Blood Pressure
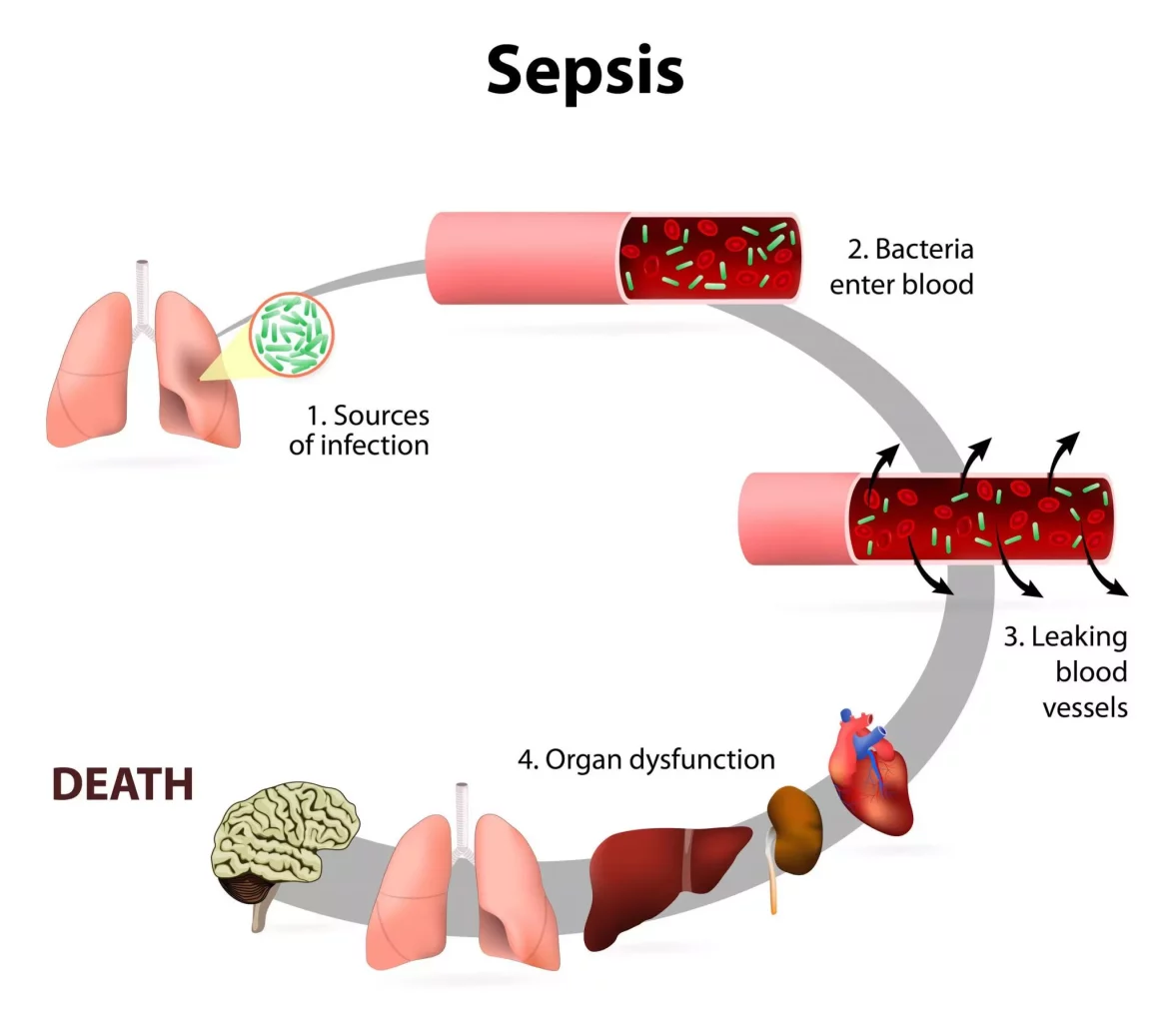
To comprehend why sepsis induces hypotension, it’s crucial to first grasp the basics of sepsis itself. Sepsis arises from an exaggerated immune response to an infection, often bacterial, but sometimes viral or fungal. This immune overreaction leads to the release of inflammatory molecules such as cytokines, which play a central role in the pathophysiology of sepsis.
Inflammatory Response and Vasodilation
One of the key mechanisms through which sepsis causes hypotension is by triggering a massive inflammatory response throughout the body. Inflammatory mediators like tumor necrosis factor-alpha (TNF-alpha), interleukins (IL-1, IL-6), and nitric oxide (NO) are released in large quantities in response to the infection. These molecules have vasodilatory effects, meaning they cause blood vessels to relax and widen.
Endothelial Dysfunction and Capillary Leak
In addition to vasodilation, sepsis also leads to endothelial dysfunction, where the cells lining blood vessels (endothelial cells) become impaired. This dysfunction contributes to capillary leak syndrome, where fluid and proteins leak from blood vessels into surrounding tissues. The loss of fluid from the circulation further reduces blood volume and exacerbates hypotension.
Impaired Cardiac Function
Another critical aspect of sepsis-induced hypotension is the impact on cardiac function. Sepsis can lead to myocardial depression, where the heart muscle becomes weakened and less effective at pumping blood. This myocardial dysfunction, coupled with the vasodilation and fluid loss mentioned earlier, contributes significantly to the drop in blood pressure seen in septic patients.
Dysregulated Immune Response and Coagulation
The immune response in sepsis is not only excessive but also dysregulated. This dysregulation can lead to abnormalities in the coagulation system, causing a condition known as disseminated intravascular coagulation (DIC). DIC further exacerbates hypotension by promoting the formation of small blood clots within blood vessels, impairing blood flow and contributing to organ dysfunction.
Impact on Organ Perfusion and Oxygen Delivery
Hypotension in sepsis has profound implications for organ perfusion and oxygen delivery. With reduced blood pressure, vital organs such as the kidneys, liver, and brain may not receive an adequate blood supply. This can lead to organ dysfunction and, if left untreated, organ failure. The decreased oxygen delivery to tissues also contributes to the development of metabolic acidosis, further complicating the clinical picture.
Clinical Management of Sepsis-Induced Hypotension
Managing hypotension in septic patients is a complex task that requires a multi-faceted approach. Prompt recognition and diagnosis of sepsis are crucial, followed by aggressive resuscitative measures. Fluid resuscitation with intravenous fluids is often the first step to address hypovolemia and improve blood pressure. However, excessive fluid administration must be avoided to prevent complications such as pulmonary edema.
Vasopressors and Inotropes
In cases where fluid resuscitation alone is insufficient to stabilize blood pressure, vasopressor medications may be used. Vasopressors like norepinephrine and vasopressin act to constrict blood vessels, raising blood pressure. Inotropes such as dobutamine can also be employed to improve cardiac contractility and output.
Targeted Antibiotics and Source Control
Addressing the underlying infection is paramount in sepsis management. Administering appropriate antibiotics based on the suspected or identified pathogen is crucial to halt the progression of the infection. Source control measures, such as draining abscesses or removing infected tissues, help eliminate the source of the infection and reduce the ongoing inflammatory response.
Conclusion
Sepsis-induced hypotension is a complex interplay of inflammatory mediators, vasodilation, endothelial dysfunction, cardiac dysfunction, and dysregulated immune responses. Understanding these mechanisms is essential for clinicians to effectively manage septic patients and improve outcomes. Early recognition, aggressive resuscitation, targeted antibiotic therapy, and source control are key components of successful sepsis management, aimed at restoring hemodynamic stability and preventing organ dysfunction.