Premature ventricular contractions (PVCs) are a common heart rhythm disorder that can cause discomfort and concern for many individuals. One puzzling aspect of PVCs is their tendency to worsen at night for some people. This phenomenon has sparked interest and research in understanding the underlying reasons behind this nighttime aggravation of PVCs.
Understanding PVCs
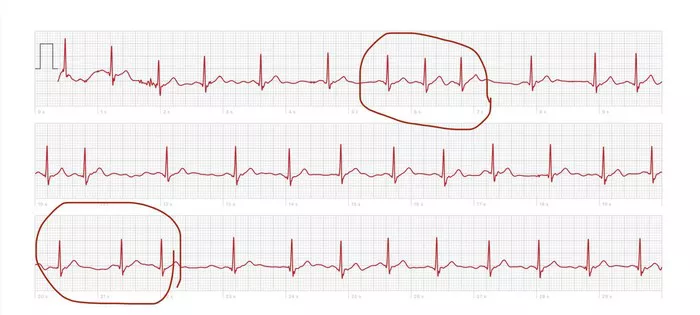
To comprehend why PVCs may intensify at night, it’s essential to first understand what PVCs are and how they occur. PVCs are abnormal heartbeats that originate in the ventricles, the lower chambers of the heart. Instead of following the normal electrical pathway through the heart’s natural pacemaker (the sinoatrial node), PVCs originate from an ectopic focus within the ventricles, causing a premature heartbeat.
Factors Contributing to Nighttime Worsening of PVCs
Several factors can contribute to the exacerbation of PVCs during nighttime hours. These factors include:
1. Hormonal Influence: Hormonal fluctuations, particularly changes in adrenaline levels, can play a role in triggering PVCs. Adrenaline, also known as epinephrine, is a hormone that is released in response to stress or excitement. During nighttime, hormonal levels can vary, potentially leading to increased adrenaline and subsequent PVCs.
2. Increased Sensitivity: Some individuals may experience increased sensitivity to PVCs at night due to factors such as reduced external stimuli and heightened awareness of bodily sensations. This heightened awareness can make PVCs feel more pronounced and bothersome during nighttime hours.
3. Changes in Heart Rate and Rhythm: Nighttime is often associated with changes in heart rate and rhythm. For example, the body’s natural circadian rhythm influences heart rate, with variations between daytime and nighttime rates. Additionally, certain sleep stages, such as REM (rapid eye movement) sleep, can lead to fluctuations in heart rate and rhythm, potentially triggering PVCs.
4. Sleep-Related Issues: Sleep disturbances or disorders, such as sleep apnea, can contribute to the worsening of PVCs at night. Sleep apnea is characterized by pauses in breathing during sleep, leading to oxygen deprivation and increased stress on the cardiovascular system, which can exacerbate PVCs.
5. Electrolyte Imbalance: Imbalances in electrolytes, such as potassium, magnesium, and calcium, can affect the heart’s electrical activity and contribute to arrhythmias like PVCs. Factors such as dietary intake, medication use, and hydration status can influence electrolyte levels and impact PVC occurrence, including worsening at night.
6. Stress and Anxiety: Emotional stress and anxiety, which can be more pronounced for some individuals during nighttime hours, can trigger PVCs. Stress activates the sympathetic nervous system, leading to the release of stress hormones like adrenaline, which can stimulate PVCs.
7. Medication Timing: The timing of certain medications, such as beta-blockers or anti-arrhythmic drugs, can influence PVC occurrence. If medication levels decrease or wear off during nighttime hours, this can potentially lead to an increase in PVC frequency.
Coping Strategies and Management
Managing PVCs that worsen at night involves a multifaceted approach that addresses potential contributing factors. Here are some strategies that individuals can consider:
1. Healthy Lifestyle: Adopting a healthy lifestyle, including regular exercise, a balanced diet, adequate hydration, and stress management techniques, can help improve overall heart health and reduce PVC frequency.
2. Sleep Hygiene: Practicing good sleep hygiene, such as maintaining a consistent sleep schedule, creating a relaxing bedtime routine, and optimizing sleep environment (e.g., comfortable mattress, dark and quiet room), can promote better sleep quality and potentially reduce nighttime PVCs.
3. Medication Management: Working closely with a healthcare provider to optimize medication management, including proper dosing and timing of medications, is crucial for individuals with PVCs.
4. Stress Reduction Techniques: Engaging in stress-reducing activities such as mindfulness meditation, deep breathing exercises, yoga, or therapy can help manage stress and anxiety levels, thereby reducing PVC triggers.
5. Monitoring and Reporting: Keeping a journal or log of PVC episodes, including their frequency, duration, and associated symptoms, can provide valuable information for healthcare providers to tailor treatment plans accordingly.
Seeking Medical Evaluation
While occasional PVCs are common and often benign, persistent or worsening PVCs, especially at night, should prompt evaluation by a healthcare professional. Diagnostic tests such as electrocardiograms (ECGs), Holter monitoring, echocardiograms, and blood tests may be recommended to assess heart function, identify underlying causes, and determine appropriate management strategies.
Conclusion
The worsening of PVCs at night can be influenced by various factors such as hormonal fluctuations, increased sensitivity, changes in heart rate and rhythm, sleep-related issues, electrolyte imbalances, stress, and medication timing. Understanding these factors and implementing appropriate coping strategies and medical management can help individuals effectively manage and reduce nighttime PVC exacerbation, promoting better heart health and overall well-being.