Hyperlipidemia type 2, also known as hypercholesterolemia, is a common metabolic disorder characterized by elevated levels of low-density lipoprotein (LDL) cholesterol in the bloodstream. This condition is a significant risk factor for cardiovascular diseases such as heart attacks and strokes. In this comprehensive article, we will delve into the details of hyperlipidemia type 2, including its causes, symptoms, diagnosis, and management strategies.
What Causes Hyperlipidemia Type 2?
Hyperlipidemia type 2 can result from various genetic and lifestyle factors. One of the primary causes is familial hypercholesterolemia (FH), an inherited condition that leads to high levels of LDL cholesterol from birth. FH is typically caused by mutations in genes responsible for cholesterol metabolism, such as the LDL receptor gene (LDLR) or the apolipoprotein B gene (APOB). Individuals with FH have a significantly increased risk of early-onset cardiovascular diseases if left untreated.
Apart from genetic factors, lifestyle choices also play a crucial role in the development of hyperlipidemia type 2. Diets high in saturated fats, trans fats, and cholesterol can contribute to elevated LDL cholesterol levels. Lack of physical activity, obesity, smoking, and excessive alcohol consumption are additional risk factors associated with this condition.
Symptoms of Hyperlipidemia Type 2
Hyperlipidemia type 2 is often asymptomatic, meaning individuals may not experience noticeable symptoms until complications such as cardiovascular diseases arise. However, some people with extremely high cholesterol levels may develop visible signs such as xanthomas, which are fatty deposits under the skin, typically around the eyes, elbows, knees, or hands. Xanthelasmas, yellowish patches on the eyelids, can also occur in individuals with hyperlipidemia.
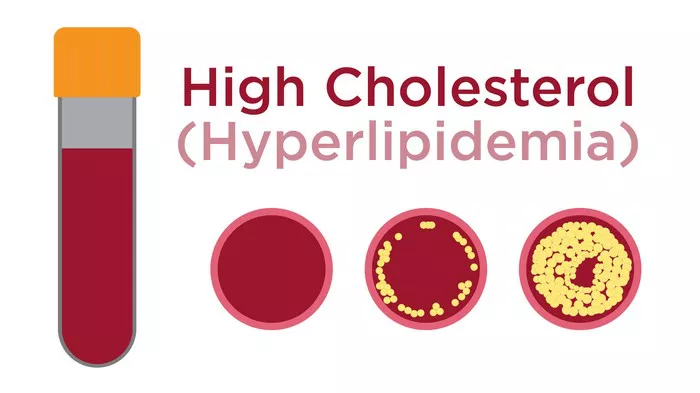
The most concerning aspect of hyperlipidemia type 2 is its association with atherosclerosis, the buildup of plaque in the arteries. This condition can lead to narrowed or blocked arteries, increasing the risk of heart attacks, strokes, and peripheral artery disease. Therefore, early detection and management of hyperlipidemia are crucial to prevent these serious complications.
Diagnosis of Hyperlipidemia Type 2
Diagnosing hyperlipidemia type 2 involves assessing lipid levels in the blood through lipid profile tests. These tests measure various lipid components, including total cholesterol, LDL cholesterol, high-density lipoprotein (HDL) cholesterol, and triglycerides. The American Heart Association recommends regular lipid screenings for adults starting at age 20 and more frequently for individuals with risk factors or a family history of hyperlipidemia or cardiovascular diseases.
Interpretation of lipid profile results is based on established guidelines that define optimal, borderline high, high, and very high levels for each lipid component. In hyperlipidemia type 2, LDL cholesterol levels are typically elevated, while HDL cholesterol levels may be normal or decreased. Triglyceride levels can also be elevated in some cases, especially in individuals with metabolic syndrome or diabetes.
Management Strategies for Hyperlipidemia Type 2
The management of hyperlipidemia type 2 aims to reduce LDL cholesterol levels and minimize the risk of cardiovascular complications. Lifestyle modifications and pharmacological interventions are key components of treatment.
Lifestyle Modifications:
1. Dietary Changes: Adopting a heart-healthy diet is crucial, focusing on foods low in saturated fats, trans fats, and cholesterol. This includes consuming more fruits, vegetables, whole grains, lean proteins, and sources of unsaturated fats such as olive oil, avocados, and nuts.
2. Regular Exercise: Engaging in regular physical activity, such as brisk walking, cycling, or swimming, helps improve lipid profiles, boost HDL cholesterol levels, and manage weight.
3. Weight Management: Maintaining a healthy weight through a combination of diet and exercise is important, as obesity can contribute to dyslipidemia and cardiovascular risk.
4. Smoking Cessation and Limiting Alcohol: Quitting smoking and limiting alcohol consumption can also improve lipid profiles and overall cardiovascular health.
Pharmacological Interventions:
1. Statins: Statin medications are the first-line treatment for hyperlipidemia type 2. They work by inhibiting the enzyme responsible for cholesterol synthesis in the liver, leading to decreased LDL cholesterol levels. Examples of statins include atorvastatin, simvastatin, and rosuvastatin.
2. Ezetimibe: Ezetimibe is another medication that can be used alone or in combination with statins to further lower LDL cholesterol levels. It works by reducing cholesterol absorption in the intestines.
3. PCSK9 Inhibitors: For individuals with familial hypercholesterolemia or those who cannot tolerate statins, PCSK9 inhibitors such as evolocumab and alirocumab may be prescribed to lower LDL cholesterol levels significantly.
4. Bile Acid Sequestrants: These medications, such as cholestyramine and colesevelam, bind to bile acids in the intestine, leading to increased bile acid excretion and reduced LDL cholesterol levels.
5. Fibrates and Niacin: Fibrates and niacin can be used to target elevated triglyceride levels and increase HDL cholesterol levels, although their use has become less common due to potential side effects and newer, more effective treatments.
Monitoring and Follow-Up:
Regular monitoring of lipid levels is essential to assess treatment effectiveness and make necessary adjustments.
Healthcare providers may also evaluate other cardiovascular risk factors such as blood pressure, blood glucose levels, and smoking status to provide comprehensive care.
Conclusion
Hyperlipidemia type 2, characterized by elevated LDL cholesterol levels, poses a significant risk for cardiovascular diseases if left untreated. Understanding the causes, symptoms, diagnosis, and management strategies for this condition is crucial for healthcare providers and individuals alike. By implementing lifestyle modifications, such as a heart-healthy diet, regular exercise, and smoking cessation, along with appropriate pharmacological interventions, such as statins and other cholesterol-lowering medications, individuals with hyperlipidemia type 2 can effectively manage their lipid levels and reduce their risk of cardiovascular complications. Regular monitoring and follow-up with healthcare providers are key components of long-term management and prevention.