Diabetes and coronary heart disease (CHD) are two interrelated health conditions that often coexist, with diabetes significantly increasing the risk of developing CHD. Understanding the mechanisms by which diabetes contributes to CHD is crucial for effective prevention and management strategies. This article explores the complex relationship between diabetes and CHD, highlighting the underlying processes and potential interventions.
Coronary heart disease remains a leading cause of morbidity and mortality worldwide, with diabetes emerging as a major risk factor for its development. In this section, we will provide an overview of both conditions and their prevalence to set the stage for understanding their interconnectedness.
Prevalence of Diabetes and CHD
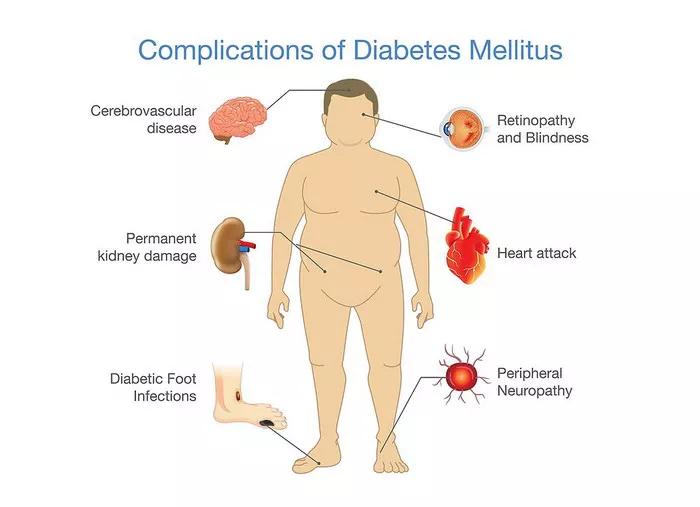
Diabetes mellitus is a chronic metabolic disorder characterized by elevated blood glucose levels, affecting millions of individuals globally. Concurrently, coronary heart disease encompasses various conditions that affect the heart’s blood vessels, such as coronary artery disease (CAD) and myocardial infarction (heart attack). The prevalence of diabetes among individuals with CHD is notably higher compared to the general population, underscoring the link between these two conditions.
Pathophysiology of Diabetes and CHD
A detailed exploration of the pathophysiological processes involved in both diabetes and CHD is essential to elucidate how diabetes contributes to the development and progression of coronary heart disease. Key mechanisms include insulin resistance, inflammation, dyslipidemia, oxidative stress, and endothelial dysfunction, all of which play integral roles in the pathogenesis of both conditions.
Insulin Resistance and Hyperglycemia
Insulin resistance, a hallmark of type 2 diabetes, leads to impaired glucose uptake by cells, resulting in elevated blood glucose levels. Prolonged hyperglycemia contributes to endothelial damage and dysfunction, promoting atherosclerosis—a major component of coronary artery disease. Moreover, hyperglycemia induces oxidative stress and inflammation, further exacerbating vascular damage and atherosclerotic plaque formation.
Dyslipidemia and Atherogenic Lipoproteins
Diabetes is often associated with dyslipidemia, characterized by elevated triglycerides, low-density lipoprotein cholesterol (LDL-C), and decreased high-density lipoprotein cholesterol (HDL-C) levels. This dyslipidemic profile promotes the formation of atherogenic lipoproteins, contributing to the initiation and progression of atherosclerosis in the coronary arteries. The interplay between diabetes, dyslipidemia, and atherosclerosis underscores the heightened cardiovascular risk in diabetic individuals.
Inflammation and Endothelial Dysfunction
Chronic inflammation and endothelial dysfunction are pivotal processes in the development of both diabetes and CHD. In diabetes, inflammatory mediators such as cytokines and chemokines are upregulated, promoting a pro-inflammatory state that accelerates vascular damage and atherogenesis. Concurrently, impaired endothelial function compromises vasodilation and promotes vasoconstriction, further contributing to coronary artery disease’s pathophysiology.
Role of Oxidative Stress
Oxidative stress, characterized by an imbalance between reactive oxygen species (ROS) production and antioxidant defenses, plays a central role in diabetic complications, including coronary heart disease. Excessive ROS generation leads to lipid peroxidation, endothelial dysfunction, and inflammatory responses within the vascular wall, perpetuating a cycle of vascular injury and atherosclerosis progression.
Interventions and Management Strategies
Given the intricate interplay between diabetes and coronary heart disease, comprehensive management strategies are essential to mitigate cardiovascular risk in diabetic individuals. This section will discuss lifestyle modifications, pharmacological interventions (including antidiabetic and cardiovascular medications), and targeted therapies aimed at addressing the underlying mechanisms linking diabetes to CHD.
Lifestyle Modifications
Healthy lifestyle habits, including regular physical activity, balanced nutrition, smoking cessation, and weight management, play pivotal roles in diabetes and CHD prevention. These interventions target modifiable risk factors such as obesity, hypertension, and dyslipidemia, contributing to improved glycemic control and cardiovascular outcomes in diabetic patients.
Pharmacological Interventions
Pharmacotherapy is a cornerstone of diabetes management, with antidiabetic agents such as metformin, sulfonylureas, insulin, and newer classes of medications like SGLT-2 inhibitors and GLP-1 receptor agonists demonstrating cardiovascular benefits beyond glycemic control. Additionally, statins, antiplatelet agents, and ACE inhibitors/ARBs are commonly prescribed to diabetic individuals with CHD to reduce cardiovascular events and mortality.
Targeted Therapies
Emerging therapies targeting specific pathways implicated in diabetes-related cardiovascular complications show promise in reducing coronary heart disease risk. These include agents targeting inflammation, oxidative stress, and endothelial function, highlighting the evolving landscape of precision medicine in diabetes and cardiovascular care.
Conclusion
In conclusion, diabetes significantly contributes to coronary heart disease through multiple interconnected mechanisms involving insulin resistance, dyslipidemia, inflammation, oxidative stress, and endothelial dysfunction. Effective management of diabetes and its associated cardiovascular risk factors is paramount in reducing the burden of coronary heart disease in diabetic individuals, emphasizing the importance of holistic approaches encompassing lifestyle modifications, pharmacological interventions, and targeted therapies.