Parkinson’s disease (PD) is a neurological disorder that primarily affects movement. It is characterized by symptoms such as tremors, stiffness, slow movement (bradykinesia), and impaired balance. However, Parkinson’s can also have non-motor symptoms that significantly impact a person’s quality of life. One such symptom is orthostatic hypotension (OH), a drop in blood pressure that occurs when a person stands up from a sitting or lying position. In this article, we will explore why Parkinson’s disease can lead to orthostatic hypotension.
Understanding Parkinson’s Disease
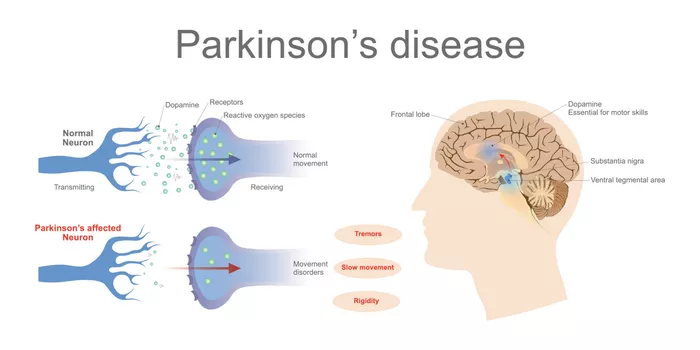
Before delving into the connection between Parkinson’s and orthostatic hypotension, it’s essential to understand the basics of Parkinson’s disease itself. PD is caused by the gradual loss of dopamine-producing cells in the brain. Dopamine is a neurotransmitter that plays a crucial role in coordinating movement. When dopamine levels drop, it leads to the motor symptoms associated with Parkinson’s.
Neurological Changes in Parkinson’s
The neurological changes in Parkinson’s extend beyond the dopamine system. The autonomic nervous system, which regulates automatic bodily functions such as blood pressure, heart rate, and digestion, can also be affected. This involvement of the autonomic nervous system contributes to various non-motor symptoms, including orthostatic hypotension.
Dopamine and Blood Pressure Regulation
One of the key mechanisms linking Parkinson’s disease to orthostatic hypotension is the role of dopamine in blood pressure regulation. Dopamine is not only involved in motor control but also influences blood vessel function and blood pressure regulation. In Parkinson’s, the loss of dopamine-producing cells can disrupt this regulatory system, leading to blood pressure fluctuations.
Autonomic Dysfunction in Parkinson’s
Parkinson’s disease can cause autonomic dysfunction, which refers to abnormalities in the autonomic nervous system’s function. This dysfunction can affect various bodily functions, including blood pressure control. In the context of orthostatic hypotension, autonomic dysfunction may result in an inadequate response to postural changes, leading to a drop in blood pressure upon standing.
Medication Effects
Another factor contributing to orthostatic hypotension in Parkinson’s is the medications used to manage the disease. Dopamine replacement therapies, such as levodopa, are commonly prescribed to alleviate motor symptoms. However, these medications can also affect blood pressure regulation, potentially exacerbating orthostatic hypotension.
Baroreflex Dysfunction
The baroreflex is a physiological mechanism that helps maintain stable blood pressure levels. It involves sensors in blood vessels that detect changes in blood pressure and trigger appropriate adjustments to keep blood pressure within a normal range. In Parkinson’s disease, dysfunction of the baroreflex system can occur, leading to inadequate compensatory responses to postural changes and contributing to orthostatic hypotension.
Reduced Sympathetic Tone
Sympathetic tone refers to the activity of the sympathetic nervous system, which plays a role in regulating blood pressure by constricting blood vessels and increasing heart rate when needed. In Parkinson’s, there can be a reduction in sympathetic tone, particularly during postural changes. This reduced sympathetic activity can lead to insufficient vasoconstriction, further contributing to orthostatic hypotension.
Vascular Dysfunction
Vascular dysfunction, characterized by impaired blood vessel function, is another factor in the development of orthostatic hypotension in Parkinson’s disease. The loss of dopamine and other neurotransmitters that help maintain vascular tone can result in abnormal vascular responses, making it challenging for the body to adjust blood pressure effectively in response to postural changes.
Neurogenic Orthostatic Hypotension
Orthostatic hypotension in Parkinson’s disease is often classified as neurogenic orthostatic hypotension (nOH). This term emphasizes the neurological origin of the blood pressure dysregulation seen in PD patients. nOH can significantly impact daily activities and increase the risk of falls and other complications.
Management Strategies
Managing orthostatic hypotension in Parkinson’s disease requires a comprehensive approach that addresses both the underlying neurological changes and the symptomatic blood pressure drops. Strategies may include:
1. Medication Adjustments: Healthcare providers may adjust Parkinson’s medications to minimize their impact on blood pressure or prescribe additional medications specifically targeting orthostatic hypotension.
2. Lifestyle Modifications: Patients can make lifestyle changes such as increasing fluid and salt intake (under medical supervision), wearing compression garments, and adopting gradual postural changes to reduce the severity of orthostatic hypotension.
3. Physical Countermeasures: Engaging in physical activities like leg exercises, leg crossing, and tensing muscles before standing can help improve blood pressure stabilization upon standing.
4. Monitoring and Awareness: Regular monitoring of blood pressure, especially during postural changes, can help identify fluctuations and guide treatment adjustments. Patients should also be educated about the symptoms of orthostatic hypotension and strategies to manage them.
Conclusion
Orthostatic hypotension is a common non-motor symptom of Parkinson’s disease, resulting from complex interactions between neurological changes, autonomic dysfunction, medication effects, and vascular factors. Understanding these mechanisms is crucial for effectively managing orthostatic hypotension and improving the quality of life for individuals living with Parkinson’s disease. Collaborative efforts between patients, caregivers, and healthcare providers are essential in developing personalized strategies to address this challenging symptom.