Ventricular tachycardia (VT) is a serious cardiac arrhythmia characterized by rapid and abnormal heartbeats originating from the ventricles of the heart. One of the key diagnostic features of VT is the wide QRS complex observed on an electrocardiogram (ECG). In this article, we delve into the mechanisms behind why the QRS complex is wide in ventricular tachycardia, exploring the pathophysiology, clinical significance, and management of this condition.
Understanding Ventricular Tachycardia
Before delving into the width of the QRS complex in ventricular tachycardia, it’s crucial to understand the basics of this arrhythmia. Ventricular tachycardia occurs when there is rapid and regular electrical activity originating from the ventricles of the heart, leading to a fast heart rate that often exceeds 100 beats per minute. This rapid rhythm can compromise cardiac output and, if left untreated, can degenerate into more life-threatening arrhythmias such as ventricular fibrillation.
Normal vs. Wide QRS Complex
In a normal sinus rhythm, the QRS complex represents ventricular depolarization, the electrical activation of the ventricles leading to ventricular contraction and subsequent ejection of blood into the systemic circulation. The duration of a normal QRS complex is typically less than 0.12 seconds (120 milliseconds) in duration.
However, in ventricular tachycardia, the QRS complex becomes wide, often exceeding 0.12 seconds in duration. This widening of the QRS complex is due to the abnormal, rapid, and disorganized electrical activation of the ventricles characteristic of ventricular tachycardia.
Pathophysiology of Wide QRS Complex in VT
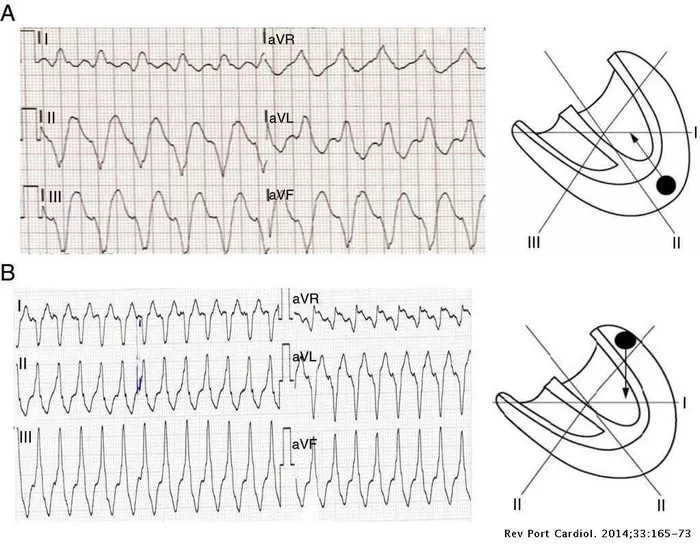
The pathophysiology of the wide QRS complex in ventricular tachycardia stems from the abnormal conduction pathways and depolarization patterns within the ventricles. Unlike the coordinated and sequential activation seen in a normal sinus rhythm, ventricular tachycardia is characterized by reentry circuits, focal ectopic beats, or other mechanisms that lead to chaotic electrical activity in the ventricles.
These abnormal electrical pathways result in delayed and heterogeneous activation of different regions of the ventricles, leading to a prolonged and widened QRS complex on the ECG. The wider the QRS complex, the greater the deviation from normal ventricular activation, reflecting the severity and complexity of the arrhythmia.
Clinical Significance of Wide QRS Complex in VT
The presence of a wide QRS complex in ventricular tachycardia has significant clinical implications. Firstly, it serves as a key diagnostic criterion for distinguishing ventricular tachycardia from other supraventricular tachycardias, which typically have narrow QRS complexes. This differentiation is crucial for guiding appropriate treatment strategies.
Secondly, the width of the QRS complex in ventricular tachycardia can provide insights into the location and extent of the ventricular activation abnormality. Certain patterns of wide QRS complexes, such as a right bundle branch block (RBBB) morphology or left bundle branch block (LBBB) morphology, can indicate specific sites of origin or conduction abnormalities within the ventricles.
Additionally, the duration of the QRS complex in ventricular tachycardia is associated with the hemodynamic stability of the patient. Prolonged and extremely wide QRS complexes may indicate compromised cardiac output and hemodynamic instability, necessitating prompt intervention and management.
Management Strategies for VT with Wide QRS Complex
The management of ventricular tachycardia with a wide QRS complex involves a multifaceted approach aimed at restoring normal cardiac rhythm, preventing recurrence, and addressing underlying cardiac pathology. Key strategies include:
1. Antiarrhythmic Medications: Pharmacological agents such as amiodarone, lidocaine, and procainamide are commonly used to stabilize cardiac rhythm and prevent further episodes of ventricular tachycardia.
2. Electrical Cardioversion: In cases of hemodynamically unstable VT or VT refractory to medications, synchronized electrical cardioversion may be performed to restore normal sinus rhythm.
3. Implantable Cardioverter-Defibrillator (ICD): Patients at high risk of recurrent ventricular tachycardia or sudden cardiac death may benefit from an ICD, which can deliver shocks or pacing therapies to terminate arrhythmic episodes.
4. Catheter Ablation: For refractory or incessant VT, catheter ablation procedures targeting the arrhythmogenic foci or critical conduction pathways within the ventricles may be considered.
5. Underlying Cardiac Evaluation: Identifying and addressing underlying cardiac conditions such as ischemic heart disease, structural heart abnormalities, or electrolyte imbalances is essential in managing ventricular tachycardia.
Conclusion
The wide QRS complex observed in ventricular tachycardia is a hallmark feature of this potentially life-threatening arrhythmia. Understanding the pathophysiology behind the widened QRS complex, its clinical significance in diagnosis and risk stratification, and the management strategies available is crucial for healthcare providers involved in the care of patients with ventricular tachycardia. Through comprehensive assessment, timely intervention, and appropriate treatment modalities, the prognosis for individuals with VT and wide QRS complexes can be significantly improved, highlighting the importance of targeted and evidence-based approaches in cardiac arrhythmia management.