Wenckebach arrhythmia, also known as Mobitz type I second-degree atrioventricular (AV) block, is a cardiac rhythm disorder characterized by a delay in the conduction of electrical impulses from the atria to the ventricles of the heart. This condition falls under the broader category of heart rhythm disturbances, which can range from benign to life-threatening. In this article, we delve into the intricacies of Wenckebach arrhythmia, including its causes, symptoms, diagnosis, treatment, and prognosis.
Causes of Wenckebach Arrhythmia
Wenckebach arrhythmia primarily results from dysfunction in the AV node, a critical component of the heart’s electrical conduction system. This dysfunction can stem from various factors, including:
1. Age-Related Changes: The aging process can lead to fibrosis and degeneration of cardiac tissues, affecting the conduction pathways.
2. Ischemic Heart Disease: Reduced blood flow to the heart muscle, often due to atherosclerosis, can disrupt electrical conduction.
3. Medications: Certain medications, such as beta-blockers, calcium channel blockers, and antiarrhythmic drugs, may interfere with AV node function.
4. Electrolyte Imbalances: Abnormal levels of potassium, magnesium, or calcium in the blood can affect cardiac conduction.
5. Structural Heart Disease: Conditions like myocardial infarction, cardiomyopathy, and valvular heart disease can contribute to AV nodal abnormalities.
Symptoms and Clinical Presentation
Patients with Wenckebach arrhythmia may present with a range of symptoms, although some individuals may remain asymptomatic. Common clinical manifestations include:
1. Palpitations: Sensations of irregular or rapid heartbeats.
2. Fatigue: Excessive tiredness or lethargy.
3. Dizziness or Lightheadedness: Feeling faint or unsteady.
4. Syncope: Episodes of fainting or loss of consciousness, though less common.
The severity and frequency of symptoms can vary widely among patients, often influenced by the underlying cause and individual cardiac health.
Diagnosis and Evaluation
Accurate diagnosis of Wenckebach arrhythmia involves a comprehensive evaluation that may include:
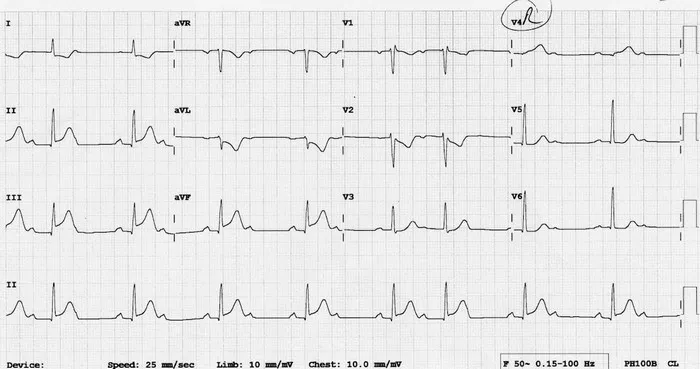
1. Electrocardiogram (ECG): A standard tool for assessing cardiac rhythm abnormalities, an ECG can reveal characteristic findings such as progressive PR interval prolongation followed by a dropped QRS complex (missing heartbeat).
2. Holter Monitoring: Continuous ECG monitoring over 24 to 48 hours can capture intermittent arrhythmias not evident during a standard ECG.
3. Echocardiography: This imaging technique provides detailed information about heart structure and function, helping identify underlying structural heart disease.
4. Exercise Stress Testing: Assessing heart rhythm during physical activity can unmask arrhythmias that occur under stress.
5. Electrophysiological Studies: Invasive procedures may be necessary in complex cases to evaluate conduction abnormalities and guide treatment decisions.
Treatment Approaches
The management of Wenckebach arrhythmia focuses on symptom control, prevention of complications, and addressing underlying causes. Treatment strategies may include:
1. Lifestyle Modifications: Adopting a heart-healthy lifestyle, including regular exercise, balanced diet, smoking cessation, and stress management, can improve overall cardiac health.
2. Medications: Antiarrhythmic drugs, beta-blockers, and calcium channel blockers may be prescribed to stabilize heart rhythm and reduce symptoms.
3. Cardiac Device Therapy: In some cases, implantation of a pacemaker or other cardiac devices may be necessary to regulate heart rate and rhythm.
4. Electrophysiology Procedures: Catheter ablation or other invasive techniques may be recommended for patients with refractory symptoms or specific arrhythmia patterns.
5. Monitoring and Follow-Up: Regular cardiac monitoring and follow-up visits are essential to assess treatment response, adjust medications, and detect any new developments promptly.
Prognosis and Complications
The prognosis of Wenckebach arrhythmia varies depending on several factors, including the underlying cause, overall cardiac health, and treatment adherence. In many cases, with appropriate management, patients can lead fulfilling lives with minimal impact from arrhythmia episodes.
However, complications may arise, particularly if the arrhythmia is left untreated or poorly controlled. These complications may include:
1. Atrioventricular Block Progression: Wenckebach arrhythmia can sometimes progress to higher degrees of AV block, necessitating more aggressive interventions.
2. Syncope and Falls: Episodes of fainting or loss of consciousness can pose risks of injury, especially in older adults.
3. Reduced Exercise Tolerance: Persistent symptoms may limit physical activity and affect quality of life.
Increased Stroke Risk: Certain arrhythmias, if associated with atrial fibrillation or other thromboembolic events, can elevate the risk of stroke.
Conclusion
In conclusion, Wenckebach arrhythmia is a distinctive form of AV block characterized by progressive PR interval prolongation and occasional dropped beats. While often manageable with appropriate medical interventions and lifestyle modifications, this condition underscores the importance of regular cardiac evaluation, prompt diagnosis, and personalized treatment plans. By addressing underlying cardiac issues and optimizing heart health, individuals with Wenckebach arrhythmia can achieve improved quality of life and reduced risk of complications.