Atrioventricular (AV) block is a cardiac conduction disorder that affects the normal electrical signal transmission between the atria (upper chambers) and ventricles (lower chambers) of the heart. This condition can vary in severity, ranging from mild disruptions in electrical conduction to complete blockage of signals, leading to potentially serious complications. In this article, we will delve into the intricacies of AV block, including its causes, symptoms, diagnosis, and treatment options.
What Causes AV Block?
AV block can occur due to various underlying causes that disrupt the electrical impulses responsible for coordinating the heart’s rhythmic contractions. Some of the common causes include:
1. Degenerative Changes: Aging can lead to degenerative changes in the heart’s conduction system, causing disruptions in signal transmission.
2. Ischemic Heart Disease: Reduced blood flow to the heart muscle due to conditions like coronary artery disease can damage the conduction pathways, resulting in AV block.
3. Myocardial Infarction (Heart Attack): A heart attack can cause damage to the heart tissue, including the conduction system, leading to AV block.
4. Cardiomyopathy: Diseases affecting the heart muscle, such as dilated cardiomyopathy or hypertrophic cardiomyopathy, can interfere with electrical conduction.
5. Medications: Certain medications, such as beta-blockers, calcium channel blockers, and antiarrhythmic drugs, may predispose individuals to AV block.
6. Electrolyte Imbalances: Abnormal levels of potassium, calcium, or magnesium in the blood can affect cardiac conduction and contribute to AV block.
7. Infections: Viral infections like myocarditis or bacterial endocarditis can inflame the heart tissue, disrupting normal electrical pathways.
8. Structural Heart Diseases: Conditions like congenital heart defects, valvular heart disease, or cardiac tumors can impact the heart’s conduction system.
Understanding AV Block Types
AV block is classified into three main types based on the severity of conduction impairment:
First-Degree AV Block:
In this type, there is a delay in the electrical signal passing from the atria to the ventricles, but all impulses eventually reach the ventricles. It is often asymptomatic and may not require specific treatment.
Second-Degree AV Block:
1. Type 1 (Wenckebach) AV Block: This type is characterized by a progressive lengthening of the PR interval (the time it takes for the electrical impulse to travel from the atria to the ventricles) until a QRS complex is dropped. It may present with symptoms like dizziness or fainting.
2. Type 2 AV Block: In this subtype, some but not all of the atrial impulses reach the ventricles. It can be further divided into Mobitz I (Wenckebach) and Mobitz II patterns, each with distinct characteristics and implications.
3. Third-Degree (Complete) AV Block: Also known as complete heart block, this type involves a complete interruption of electrical signals between the atria and ventricles. As a result, the atria and ventricles beat independently, leading to a slower heart rate and potential symptoms like fatigue, dizziness, or even syncope (fainting).
Recognizing Symptoms and Clinical Presentation
The symptoms of AV block can vary depending on the type and severity of the blockage. Some individuals may remain asymptomatic, especially in first-degree AV block or mild cases. However, as the degree of blockage increases, symptoms may become more noticeable. Common symptoms include:
1. Palpitations: Sensations of irregular or skipped heartbeats.
2. Fatigue: Feeling tired or lacking energy, especially during physical activity.
3. Dizziness or Lightheadedness: A sensation of feeling faint or woozy.
4. Syncope (Fainting): Loss of consciousness, which can occur in severe cases of AV block.
5. Chest Pain: Discomfort or pressure in the chest, although this symptom is less common with AV block alone.
6. Shortness of Breath: Difficulty breathing, especially during exertion.
It is important to note that some individuals with AV block may not experience any symptoms until the condition progresses or is triggered by specific factors such as increased physical activity or emotional stress.
Diagnosing AV Block
Diagnosing AV block involves a comprehensive evaluation that may include the following:
1. Medical History and Physical Examination: Your healthcare provider will review your medical history and conduct a physical exam to assess your heart rate, rhythm, and overall cardiovascular health.
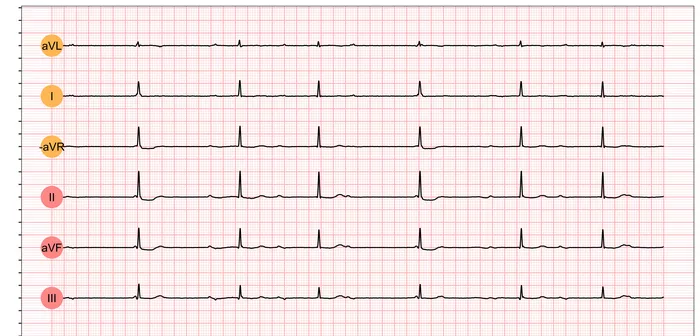
2. Electrocardiogram (ECG or EKG): This non-invasive test records the electrical activity of your heart and can detect abnormalities in the conduction system, including AV block.
3. Holter Monitor: For individuals with intermittent symptoms, a Holter monitor may be used to record continuous ECG data over a 24-hour period or longer, capturing any episodes of AV block.
4. Event Monitor: Similar to a Holter monitor, an event monitor is worn for a longer duration and is activated by the individual when symptoms occur, allowing for the recording of specific episodes.
5. Echocardiogram: This imaging test uses sound waves to create a detailed picture of the heart’s structure and function, helping assess for any underlying structural abnormalities or heart muscle issues.
6. Stress Test: In some cases, a stress test may be performed to evaluate how the heart responds to physical exertion and detect any conduction abnormalities that may become apparent during exercise.
7. Electrophysiological Studies (EPS): In complex cases or when planning for specialized treatments like pacemaker implantation, EPS may be conducted to assess the heart’s electrical pathways in detail.
Treatment Options for AV Block
The treatment approach for AV block depends on several factors, including the type and severity of the blockage, the presence of symptoms, and the individual’s overall health status. Treatment options may include:
Observation and Monitoring:
In cases of first-degree AV block or asymptomatic second-degree AV block, close observation without immediate intervention may be appropriate. Regular follow-up appointments and monitoring of symptoms and ECG findings are essential.
Medications:
1. Atropine: This medication may be administered to increase heart rate in certain types of AV block, particularly if there is symptomatic bradycardia.
2. Beta-Blockers or Calcium Channel Blockers: These medications may be prescribed cautiously in selected cases to manage heart rate or rhythm disturbances.
Temporary Cardiac Pacing:
1. Transcutaneous Pacing (TCP): External pacing can be initiated in emergency situations to temporarily support the heart’s rhythm until definitive treatment is available.
2. Transvenous Pacing: A temporary pacing wire can be inserted through a vein into the heart, providing short-term pacing support as needed.
3. Permanent Pacemaker Implantation: For individuals with symptomatic third-degree AV block or certain types of second-degree AV block (e.g., Mobitz II), permanent pacemaker placement is often recommended. A pacemaker is a small device implanted under the skin, usually in the chest area, that delivers electrical impulses to maintain a regular heart rhythm.
4. Lifestyle Modifications and Risk Factor Management: Although not a direct treatment for AV block, addressing underlying risk factors such as hypertension, diabetes, smoking cessation, and maintaining a healthy weight can improve overall cardiovascular health and potentially minimize the progression of conduction system diseases.
Living with AV Block
Living with AV block, particularly if it requires treatment such as a pacemaker, involves adapting to certain lifestyle considerations and ensuring regular follow-up with a healthcare provider. Pacemaker recipients will need to have periodic device checks to ensure it is functioning correctly and may need to avoid strong magnetic fields or activities that could disrupt the device. Despite these considerations, many individuals with AV block lead active, normal lives with appropriate management and care.
Conclusion
Atrioventricular block represents a spectrum of disorders that can impact the heart’s ability to conduct electrical signals efficiently. Through early detection, comprehensive evaluation, and tailored treatment strategies, individuals with AV block can achieve optimal outcomes. Advances in cardiac diagnostics, pacing technologies, and therapeutic interventions continue to improve the quality of life for those affected by this condition. As our understanding of AV block deepens, so too will our ability to provide effective, patient-centered care for those living with this cardiac conduction disorder.