An echocardiogram is a crucial diagnostic tool used in cardiology to assess the structure and function of the heart. This non-invasive imaging technique employs sound waves to create detailed images of the heart’s chambers, valves, and blood flow patterns. While an echocardiogram is primarily used to evaluate various cardiac conditions, including heart murmurs, valve disorders, and congenital heart defects, it can also provide valuable insights into the presence of blockages in the coronary arteries.
How Does an Echocardiogram Work?
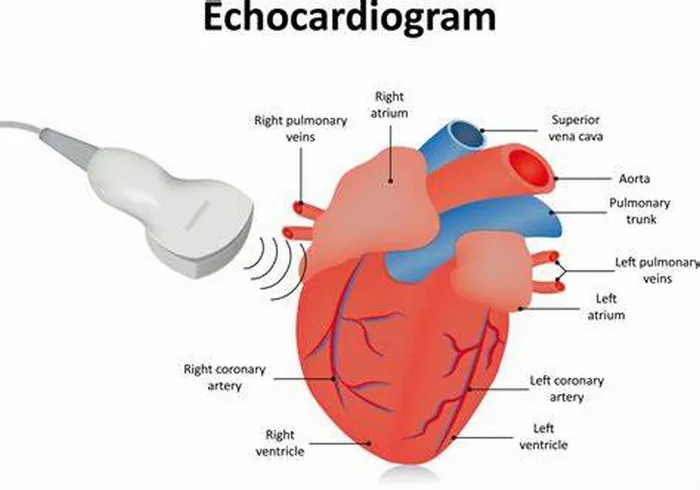
Before delving into what an echocardiogram can reveal about blockages, it’s essential to understand how this imaging modality works. During an echocardiogram, a transducer, which emits and receives sound waves, is placed on the chest overlying the heart. These sound waves travel through the chest wall and are reflected back by the heart’s structures. The returning echoes are then converted into real-time images displayed on a monitor, allowing healthcare providers to visualize the heart’s anatomy and function.
Detecting Blockages with Echocardiography
While echocardiography is not the primary method for directly visualizing coronary artery blockages, it can indirectly provide valuable information about their presence and potential impact on cardiac function. Here are several ways in which an echocardiogram can help detect blockages:
1. Assessment of Cardiac Function: One of the primary indications for an echocardiogram is to evaluate the overall function of the heart. This includes assessing the pumping ability of the heart muscle (ejection fraction), the thickness of the heart walls (wall motion abnormalities), and the presence of any structural abnormalities. Significant blockages in the coronary arteries can lead to impaired heart function, which may manifest as reduced ejection fraction or abnormal wall motion on echocardiography.
2. Evaluation of Regional Wall Motion Abnormalities: Coronary artery blockages can cause ischemia (reduced blood flow) in specific regions of the heart muscle. This ischemia can result in abnormal motion or contraction of these affected heart segments, known as regional wall motion abnormalities. Echocardiography can detect these abnormalities by visualizing the movement of different heart segments during each cardiac cycle. Areas with reduced or paradoxical motion may indicate the presence of blockages in the coronary arteries supplying those regions.
3. Detection of Indirect Signs: While echocardiography cannot directly visualize coronary arteries or their blockages, it can detect indirect signs suggestive of coronary artery disease (CAD). These signs include the presence of left ventricular hypertrophy (LVH), diastolic dysfunction, or evidence of prior heart attacks (myocardial infarctions). LVH, for example, can result from chronic hypertension, which is a significant risk factor for CAD and coronary artery blockages.
4. Assessment of Valvular Function: In addition to evaluating the coronary arteries and heart muscle, an echocardiogram assesses the function of heart valves. Valvular disorders, such as aortic stenosis or mitral regurgitation, can coexist with CAD and may provide indirect clues about the presence of coronary artery blockages. For instance, aortic stenosis often occurs in conjunction with CAD due to shared risk factors such as age and atherosclerosis.
5. Integration with Other Imaging Modalities: While echocardiography provides valuable information, it is often integrated with other imaging modalities for a comprehensive evaluation of CAD and coronary artery blockages. Techniques such as stress echocardiography, where the heart is stressed (e.g., through exercise or pharmacological agents) during imaging, can assess for inducible ischemia and identify areas of the heart at higher risk due to significant blockages.
Limitations and Considerations
It’s important to note that while echocardiography can provide valuable insights into the presence of coronary artery blockages, it is not the definitive diagnostic tool for directly visualizing these blockages. For a more detailed assessment of coronary anatomy and the extent of blockages, invasive procedures such as coronary angiography are typically performed. Coronary angiography involves inserting a catheter into the coronary arteries and injecting contrast dye to visualize any blockages or narrowing directly.
Additionally, echocardiography’s ability to detect blockages may vary depending on factors such as the location and severity of the blockages, the presence of collateral circulation, and the individual patient’s cardiac anatomy and physiology. Interpretation of echocardiographic findings in the context of clinical history, symptoms, and other diagnostic tests is essential for accurate diagnosis and management of coronary artery disease.
Conclusion
While an echocardiogram is not the primary method for directly visualizing coronary artery blockages, it plays a crucial role in evaluating cardiac structure, function, and indirect signs suggestive of coronary artery disease. By assessing cardiac function, detecting regional wall motion abnormalities, evaluating valvular function, and integrating with other imaging modalities, echocardiography contributes to a comprehensive assessment of patients with suspected CAD and helps guide further diagnostic and treatment strategies.