Atrial fibrillation (AFib) is an irregular and often very rapid heart rhythm. An irregular heart rhythm is called an arrhythmia. AFib can lead to blood clots in the heart. The condition also increases the risk of stroke, heart failure and other heart-related complications.
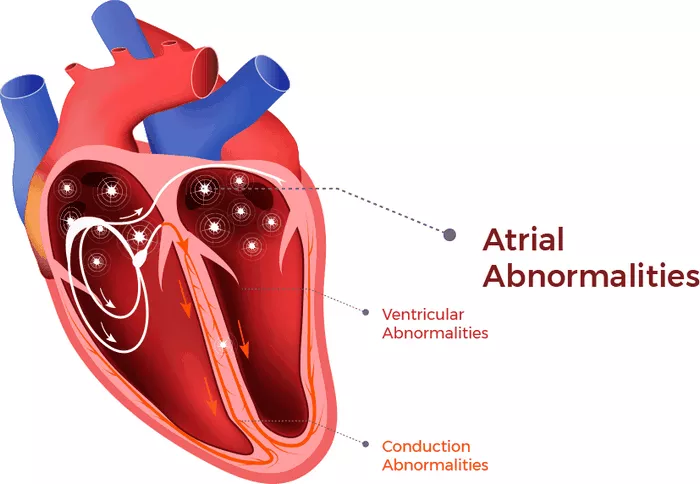
During atrial fibrillation, the heart’s upper chambers — called the atria — beat chaotically and irregularly. They beat out of sync with the lower heart chambers, called the ventricles. For many people, AFib may have no symptoms. But AFib may cause a fast, pounding heartbeat, shortness of breath or light-headedness.
Episodes of atrial fibrillation may come and go, or they may be persistent. AFib itself usually isn’t life-threatening. But it’s a serious medical condition that needs proper treatment to prevent stroke.
Treatment for atrial fibrillation may include medicines, therapy to shock the heart back to a regular rhythm and procedures to block faulty heart signals.
A person with atrial fibrillation also may have a related heart rhythm problem called atrial flutter. The treatments for AFib and atrial flutter are similar.
Symptoms
Symptoms of AFib may include:
- Feelings of a fast, fluttering or pounding heartbeat, called palpitations.
- Chest pain.
- Dizziness.
- Fatigue.
- Lightheadedness.
- Reduced ability to exercise.
- Shortness of breath.
- Weakness.
What Is The Best Medication for Atrial Fibrillation (AFib)?
Atrial fibrillation (AFib) is a common cardiac arrhythmia characterized by an irregular and often rapid heart rate. It can lead to various complications, including stroke, heart failure, and other heart-related issues. Managing AFib involves controlling the heart rate, preventing blood clots, and addressing the underlying rhythm disturbance. The choice of medication for AFib depends on several factors, including the patient’s overall health, the presence of other medical conditions, and the specific characteristics of their AFib.
See Also: How Does Myocardial Infarction Cause Arrhythmia
Beta-blockers:
Examples:Metoprolol, Atenolol, Bisoprolol, Carvedilol
Mechanism:These medications work by blocking the effects of adrenaline on the heart, slowing the heart rate.
Indications: Suitable for patients with coexisting conditions such as hypertension or heart failure.
Calcium channel blockers:
Examples: Diltiazem, Verapamil
Mechanism: These drugs block calcium entry into the heart muscle cells, leading to a slower heart rate.
Indications: Often used in patients who cannot tolerate beta-blockers.
See Also: Can Arrhythmia Cause Weight Loss
Antiarrhythmic Drugs:
Class I Antiarrhythmics:
Examples: Flecainide, Propafenone
Mechanism: Block sodium channels, stabilizing the cardiac cell membrane and reducing excitability.
Indications: Effective in maintaining sinus rhythm in patients without structural heart disease.
Class III Antiarrhythmics:
Examples: Amiodarone, Dofetilide, Sotalol
Mechanism: Block potassium channels, prolonging the action potential and refractory period.
Indications: Amiodarone is often used for its efficacy in maintaining sinus rhythm, though it has a broad side effect profile. Sotalol combines beta-blocker properties with antiarrhythmic effects.
Class IC Antiarrhythmics:
Examples: Flecainide, Propafenone
Mechanism: These medications work by blocking sodium channels in the heart, which helps maintain a normal rhythm.
Indications: These are typically used in patients without structural heart disease.
Anticoagulation Therapy
Patients with AFib are at an increased risk of stroke due to the potential formation of blood clots in the atria.
Anticoagulation therapy is crucial for preventing thromboembolic events.
Warfarin:
Mechanism: Inhibits vitamin K-dependent clotting factors.
Indications: Requires regular monitoring of INR (International Normalized Ratio) to ensure therapeutic levels.
Direct Oral Anticoagulants (DOACs):
Examples: Dabigatran, Rivaroxaban, Apixaban, Edoxaban
Mechanism: Directly inhibit specific clotting factors (thrombin or factor Xa).
Indications: Preferred over warfarin for many patients due to fewer dietary restrictions and no need for regular blood monitoring.
Understanding Atrial Fibrillation And Its Management
AFib is the most common type of treated heart arrhythmia. It is characterized by a rapid, irregular heartbeat that can lead to blood clots, stroke, heart failure, and other heart-related complications.
The Role of Medication in AFib Treatment
Medications for AFib serve three primary purposes: to control heart rate, manage heart rhythm, and prevent blood clots.
The best medication for an individual depends on their specific health profile, including age, underlying health conditions, and the severity of AFib.
Exploring AFib Medications
Rate Control Medications
Beta-blockers and calcium channel blockers are commonly used to control the heart rate in AFib patients. They help slow the heartbeat, reducing the risk of complications.
Rhythm Control Medications
These medications aim to restore and maintain a normal heart rhythm. They include sodium channel blockers and potassium channel blockers, each with its specific considerations and side effects.
Anticoagulants
Anticoagulants or blood thinners, such as warfarin and newer options like dabigatran and rivaroxaban, are crucial in preventing blood clots and stroke in AFib patients.
Comparing Medications for AFib
No single medication is best for all AFib patients. The choice of medication is influenced by individual health factors, potential side effects, and the specific goals of treatment.
Emerging Treatments And Research
Ongoing research into AFib treatments promises new medications and therapies. These developments have the potential to offer more effective management with fewer side effects.
Lifestyle And Supplementary Management
Alongside medication, lifestyle changes such as diet, exercise, and avoiding alcohol and caffeine can significantly impact AFib management.
The Importance of Consultation with Healthcare Providers
Choosing the best medication for AFib is a decision that should be made with a healthcare provider, tailored to the individual’s health needs and circumstances.
Conclusion
While there is no one-size-fits-all answer to the best medication for AFib, understanding the options available is the first step toward effective management. Consulting with healthcare professionals, considering personal health profiles, and staying informed about new treatments are key to navigating AFib treatment successfully.