In the fast-paced modern world, stress has become an unavoidable aspect of daily life for many individuals. From demanding work schedules to personal challenges and societal pressures, the effects of stress can permeate various facets of our existence, including our cardiovascular health. In this article, we embark on a journey to unravel the intricate relationship between psychological stress and heart arrhythmias, exploring the mechanisms by which stress may contribute to the development and exacerbation of these cardiac rhythm disorders.
What Are The Characteristics And Manifestations of Cardiac Arrhythmias?
Heart arrhythmias encompass a diverse array of cardiac rhythm disturbances characterized by abnormalities in the rate, rhythm, or conduction of electrical impulses within the heart. These disturbances can manifest as tachyarrhythmias (rapid heart rhythms), bradyarrhythmias (slow heart rhythms), or irregular heart rhythms such as atrial fibrillation. While arrhythmias can arise from a myriad of factors, including structural heart disease, electrolyte imbalances, and genetic predisposition, the potential role of psychological stress in precipitating or exacerbating these conditions warrants careful consideration.
Can Mental Stress Worsen Cardiac Arrhythmias?
Mental stress can increase the risk of arrhythmia, and the latest research shows that it can also increase the recurrence rate and mortality of heart disease and cause many cardiovascular problems.
Mental stress not only causes cardiovascular disease, but also causes mental and psychological problems.
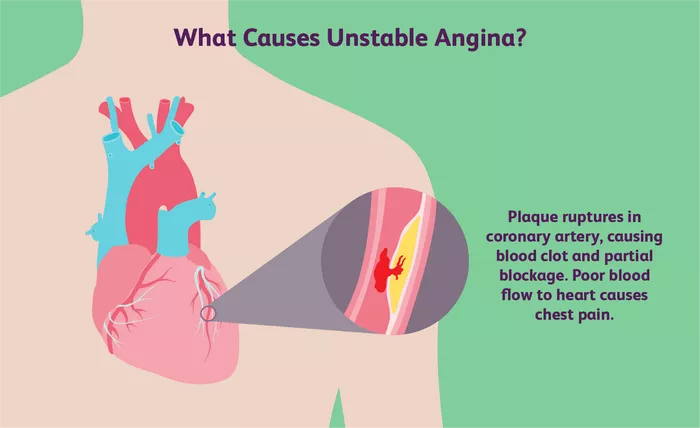
When people are under excessive mental stress, it can also lead to myocardial ischemia. This is because under excessive stress, the blood flow through the heart is reduced, so the myocardium cannot get enough oxygen, which will produce a series of cardiovascular diseases. event.
The Stress Response And The Autonomic Nervous System
The body’s response to stress is orchestrated by the autonomic nervous system (ANS), a complex network of nerves that regulates involuntary bodily functions such as heart rate, blood pressure, and respiration. In times of stress, the sympathetic branch of the ANS is activated, triggering the “fight or flight” response characterized by the release of stress hormones such as adrenaline and noradrenaline. These physiological changes prepare the body to confront or flee from perceived threats, enhancing alertness, energy mobilization, and cardiovascular function.
Impact of Stress on Cardiac Electrophysiology
Psychological stress can exert profound effects on cardiac electrophysiology, influencing the generation and propagation of electrical impulses within the heart. Sympathetic activation during periods of stress can enhance myocardial excitability and automaticity, predisposing to the development of ectopic beats, premature atrial or ventricular contractions, and other arrhythmogenic mechanisms. Additionally, stress-induced alterations in autonomic tone may disrupt the delicate balance between sympathetic and parasympathetic influences on cardiac conduction, increasing the risk of arrhythmia occurrence or recurrence.
Stress and Triggering of Arrhythmia Episodes
While stress alone may not directly cause arrhythmias in individuals without underlying cardiac pathology, it can serve as a potent trigger for arrhythmia episodes in susceptible individuals. For individuals with preexisting arrhythmia substrates, such as atrial fibrillation or ventricular tachycardia, acute stressors or chronic psychological stressors may precipitate arrhythmia onset or exacerbate existing arrhythmia burden. Common triggers include acute emotional stress, work-related stress, interpersonal conflicts, financial worries, and major life events.
What Is the Mechanisms Linking Stress to Arrhythmia Pathophysiology?
Several mechanisms have been proposed to elucidate the link between stress and arrhythmia pathophysiology, including:
Activation of the sympathetic nervous system and release of stress hormones, leading to increased myocardial excitability and arrhythmogenesis.
Promotion of pro-inflammatory and prothrombotic states, contributing to endothelial dysfunction, oxidative stress, and atrial remodeling.
Disruption of autonomic balance and heart rate variability, predisposing to electrical instability and susceptibility to arrhythmias.
Psychological factors such as anxiety, depression, and emotional distress, which can impact cardiac electrophysiology through neurohormonal pathways and psychosocial mechanisms.
Clinical Implications And Management Strategies
Recognition of the role of stress in arrhythmia pathophysiology has important clinical implications for risk assessment, arrhythmia management, and patient education. Healthcare providers should conduct comprehensive evaluations of psychosocial stressors and psychological factors in individuals with arrhythmias, incorporating stress management strategies into multidisciplinary treatment plans.
Lifestyle modifications, relaxation techniques, cognitive-behavioral therapies, and mindfulness-based interventions may be beneficial in reducing stress-related arrhythmia triggers and improving overall cardiovascular health.
Conclusion
In conclusion, the intricate interplay between psychological stress and heart arrhythmias underscores the importance of adopting a holistic approach to cardiovascular care that addresses both physiological and psychosocial determinants of disease.
FAQs
What does a heart rate below 60 mean?
A heart rate below 60 beats per minute (bpm) is typically considered bradycardia, which may indicate that the heart is beating slower than normal. While bradycardia can be a normal finding in athletes or during sleep, it can also be associated with certain medical conditions, medication side effects, or disruptions in the heart’s electrical conduction system. Symptoms of bradycardia may include dizziness, fatigue, weakness, fainting, or shortness of breath.
How do you know if you have symptoms of heart disease?
Symptoms of heart disease can vary depending on the specific condition and its severity. Common symptoms may include chest pain or discomfort (angina), shortness of breath, fatigue, palpitations, dizziness, lightheadedness, swelling in the legs, ankles, or abdomen, and symptoms of heart failure such as coughing, wheezing, or difficulty lying flat. It’s essential to seek medical evaluation if experiencing any concerning symptoms, especially if they are new, persistent, or severe.
What can’t people with heart problems eat?
Individuals with heart problems should follow a heart-healthy diet that emphasizes fruits, vegetables, whole grains, lean proteins, and healthy fats while minimizing intake of saturated fats, trans fats, cholesterol, sodium, and added sugars. Foods to limit or avoid may include processed meats, fried foods, sugary beverages, high-sodium foods, and foods high in saturated or trans fats. It’s essential to consult with a healthcare provider or registered dietitian for personalized dietary recommendations.
What are the symptoms before sudden death?
Sudden death may occur unexpectedly and without warning, but in some cases, there may be warning signs or symptoms. These may include chest pain or discomfort, palpitations, shortness of breath, dizziness, lightheadedness, fainting, or sudden collapse. However, sudden death can also occur without preceding symptoms, particularly in cases of sudden cardiac arrest or arrhythmias such as ventricular fibrillation. Prompt recognition of symptoms and access to emergency medical care are crucial for improving outcomes in cases of sudden cardiac events.