Arrhythmia, or irregular heart rhythm, is a common cardiac condition that affects millions of individuals worldwide. Understanding what arrhythmia entails and how it is diagnosed is crucial for timely intervention and optimal management. In this comprehensive article, we will delve into the intricacies of arrhythmia, exploring its definition, types, causes, symptoms, and the diagnostic modalities used by healthcare professionals to identify and assess this cardiac disturbance.
What Is Arrhythmia?
Define arrhythmia as any deviation from the normal rhythm or rate of the heartbeat, encompassing both slow (bradycardia) and fast (tachycardia) heart rhythms, as well as irregular heartbeats.
the significance of arrhythmia in disrupting the heart’s ability to pump blood effectively and potentially leading to complications such as stroke, heart failure, or sudden cardiac arrest.
What Types of Arrhythmias Are There?
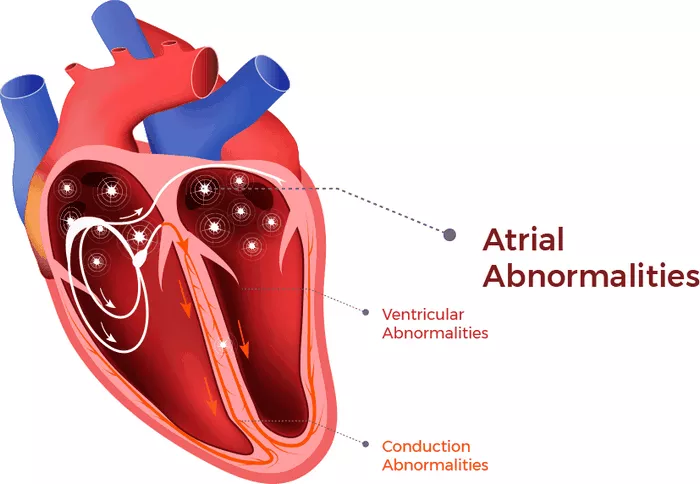
Arrhythmias can be divided into the following categories based on the origin of the impulse:
Arrhythmias caused by irregular impulses from the sinoatrial node are called “sinus arrhythmias” and mainly include:
- sinus tachycardia
- sinus bradycardia
- sinus arrhythmia
- sinus arrest, etc.
If the origin of the impulse is not the sinoatrial node, it is called an “ectopic rhythm.” If the impulse occurs in the atrium, it is called “atrial arrhythmia”
If it occurs within the ventricles, it is called a “ventricular arrhythmia.” There are many types of ectopic rhythms, including:
- Various types of premature beats (atrial, ventricular)
- Various types of tachycardia (atrial, supraventricular, ventricular)
- Flutter (atrial flutter, ventricular flutter)
- Fibrillation (atrial fibrillation, ventricular fibrillation)
According to the different heart rate, it can be divided into two categories: bradycardia and tachyarrhythmia.
Sick sinus syndrome, atrioventricular block, etc. are “bradyarrhythmias”. Bradyarrhythmias generally refer to heartbeats less than 60 beats per minute or cardiac arrest or long pauses, including sick sinus syndrome and atrioventricular block.
Premature beats, tachycardia, flutter, tremor, etc. are “tachyarrhythmias.” The development pattern of tachyarrhythmia, taking atrial arrhythmia as an example.
Causes And Risk Factors
Identify the underlying causes and risk factors associated with arrhythmia, such as coronary artery disease, hypertension, heart valve disorders, electrolyte imbalances, thyroid dysfunction, and congenital heart defects.
Highlight lifestyle factors that may contribute to the development of arrhythmias, including excessive alcohol consumption, smoking, illicit drug use, and chronic stress.
How Is Arrhythmia Diagnosed?
Feel for pulse: The easiest way to initially diagnose arrhythmia is to feel for pulse. A pulse that is too fast, too slow, or irregular often indicates the occurrence of arrhythmia.
Electrocardiogram: records the beating pattern of the heart, but the recording time is short. The ECG is an important basis for diagnosis when an arrhythmia occurs, but most arrhythmias are paroxysmal. If the patient does not have an attack when the patient sees the doctor, the ECG may still be normal.
Holter monitoring (Holter): Continuously records the beating of the heart for 24 to 48 hours, which is more helpful in catching arrhythmias.
Esophageal electrophysiological examination: The catheter is sent into the esophagus through the nasal cavity to stimulate the heart and record the electrical activity of the heart. For further diagnosis of complex arrhythmias, testing cardiac function is of great significance.
Intracardiac electrophysiological examination: The electrode catheter is sent into the heart chamber through the blood vessel. The electrode catheter can:
Record signals: feel the electrical activity in different parts of the heart and detect the conduction speed of electrical impulses
Cardiac pacing: sends weak electrical stimulation to pace the heart and induce certain arrhythmias, allowing doctors to determine the origin and type of arrhythmias under artificially controlled conditions and help choose the best treatment measures
Cardiac magnetic resonance examination: to determine whether there are organic lesions in the heart, such as dilated, hypertrophic cardiomyopathy, etc.
Additional Diagnostic Tests
Describe complementary diagnostic tests that may be utilized to further evaluate arrhythmias, such as ambulatory Holter monitoring, event monitoring, exercise stress testing, echocardiography, cardiac MRI, electrophysiology studies, and cardiac biomarker testing.
Highlight the indications, advantages, and limitations of each diagnostic modality in assessing arrhythmia and guiding treatment decisions.
Differential Diagnosis
Address the importance of distinguishing arrhythmias from other cardiac and non-cardiac conditions that may present with similar symptoms, such as anxiety, panic attacks, syncope, or non-cardiac chest pain.
Discuss clinical considerations and diagnostic criteria used to differentiate arrhythmias from other potential causes of symptoms.
Treatment Implications
Emphasize the significance of accurate diagnosis in guiding appropriate treatment strategies for arrhythmia management.
Discuss the importance of individualized treatment plans tailored to each patient’s specific arrhythmia subtype, symptoms, underlying health conditions, and lifestyle factors.
Prognosis And Follow-Up
Provide insights into the prognosis of arrhythmia based on factors such as the type, severity, and response to treatment.
Stress the importance of regular follow-up appointments, monitoring, and adherence to treatment recommendations to optimize outcomes and prevent complications.
Conclusion
Arrhythmia is a common clinical abnormality, generally related to conduction disorders. Under the influence of conduction disorders, the frequency and rhythm of heart beats are abnormal, so arrhythmias occur. Moreover, arrhythmias are also an important group of cardiovascular and cerebrovascular diseases, which can occur alone or together with other cardiovascular diseases.
FAQs
How to Correctly Evaluate the Side Effects of Antiarrhythmic Drugs?
Establish a structured approach to monitor and assess potential side effects of antiarrhythmic drugs, including baseline evaluation and ongoing monitoring during treatment.
Educate patients about potential side effects associated with specific antiarrhythmic medications and encourage them to report any new or worsening symptoms promptly.
Utilize clinical guidelines and recommendations to guide the selection and dosing of antiarrhythmic drugs, taking into account patient-specific factors such as age, comorbidities, renal function, and concomitant medications.
Monitor patients regularly for known side effects of antiarrhythmic drugs, such as proarrhythmia, QT prolongation, bradycardia, hypotension, pulmonary toxicity, hepatotoxicity, and adverse drug interactions.
Which Groups are Susceptible to Cardiac Arrhythmias?
Individuals with underlying heart conditions or structural heart disease, such as coronary artery disease, heart failure, cardiomyopathy, valvular heart disease, congenital heart defects, or prior myocardial infarction, are at increased risk of developing cardiac arrhythmias.
Elderly individuals, especially those with age-related changes in cardiac conduction and autonomic function, may be more susceptible to arrhythmias, including atrial fibrillation, atrial flutter, and bradyarrhythmias
Patients with electrolyte imbalances, such as hypokalemia, hyperkalemia, hypomagnesemia, or hypercalcemia, are prone to developing arrhythmias due to disturbances in cardiac ion channels and electrical conduction.
Individuals with autonomic nervous system disorders, such as autonomic neuropathy, Parkinson’s disease, or diabetes mellitus, may experience dysregulation of heart rate and rhythm, predisposing them to arrhythmias.
Athletes and physically active individuals, particularly endurance athletes, may develop arrhythmias such as atrial fibrillation or ventricular ectopy due to structural remodeling and autonomic modulation of the heart associated with intense exercise training.
Patients with a history of substance abuse, including alcohol, stimulants (e.g., cocaine, amphetamines), or certain medications (e.g., psychotropic drugs, QT-prolonging agents), may be at increased risk of developing arrhythmias due to direct cardiac toxicity or electrolyte disturbances.
What are Sinus Rhythm and Sinus Arrhythmia?
Sinus rhythm: refers to the normal heart rhythm originating from the sinoatrial (SA) node, the heart’s natural pacemaker, with regular atrial depolarization followed by coordinated ventricular contraction. Sinus rhythm typically exhibits a regular rate (60-100 beats per minute in adults at rest) and a normal sequence of P waves, QRS complexes, and T waves on the electrocardiogram (ECG).
Sinus arrhythmia: it is a variation of sinus rhythm characterized by slight irregularity in the heart rate, with subtle changes in the timing of atrial depolarization and resulting RR intervals on the ECG. Sinus arrhythmia is commonly observed during respiration, with heart rate increasing during inspiration and decreasing during expiration due to fluctuations in vagal tone.