As a cardiologist, I often encounter patients who express concerns about the signs and symptoms of right-sided congestive heart failure (CHF). Understanding these clinical manifestations is crucial for early recognition, diagnosis, and management of this condition. In this article, we will explore the various signs of right-sided congestive heart failure, shedding light on the pathophysiology, clinical presentation, diagnostic evaluation, and treatment considerations.
What Is Congestive Heart Failure?
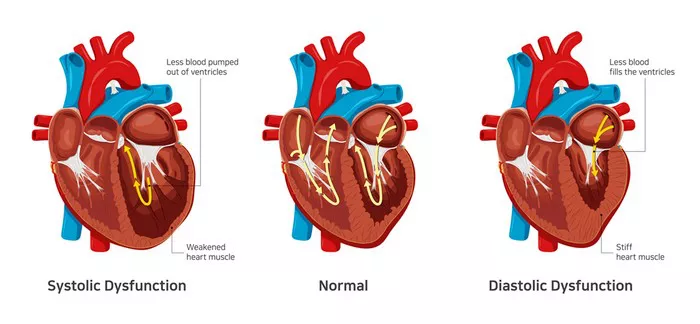
It refers to cardiac systolic and/or diastolic dysfunction caused by any factor, impaired cardiac ejection capacity, significant reduction in ejection volume, resulting in ventricular congestion and increased ventricular filling pressure, resulting in insufficient blood perfusion of our body tissues and organs. , unable to meet the needs of our body, resulting in a series of symptoms such as difficulty breathing and edema.
What Is Signs of Right-Sided Congestive Heart Failure?
The signs of right-sided congestive heart failure can vary depending on the underlying etiology, disease severity, and individual patient characteristics. However, several hallmark signs are commonly observed in clinical practice:
Peripheral Edema: One of the classic signs of right-sided CHF is peripheral edema, particularly in the lower extremities. Patients may notice swelling in the ankles, feet, and legs, which is often bilateral and may worsen throughout the day, especially after prolonged periods of standing or sitting.
Ascites: In more severe cases of right-sided CHF, fluid accumulation may extend beyond the lower extremities to involve the abdominal cavity, leading to the development of ascites. Ascites presents as abdominal distension, discomfort, and increased girth, and may be associated with symptoms such as early satiety and difficulty breathing.
Hepatomegaly: Congestion of the hepatic circulation can result in hepatomegaly, or enlargement of the liver. Clinically, this may manifest as right upper quadrant tenderness or fullness on physical examination. Elevated liver enzymes and abnormal liver function tests may also be observed in laboratory studies.
Jugular Venous Distension: Examination of the jugular venous pulsation can provide valuable insights into the hemodynamic status of patients with right-sided CHF. Jugular venous distension, or visible pulsations of the jugular veins above the clavicle, may indicate elevated right atrial pressure and venous congestion.
Hepatojugular Reflux: This maneuver involves applying sustained pressure to the liver or abdomen while observing for an increase in jugular venous pressure. A positive hepatojugular reflux test, characterized by a sustained rise in jugular venous pressure, suggests impaired right ventricular function and venous congestion.
Pleural Effusions: The accumulation of fluid in the pleural space, known as pleural effusion, can occur secondary to right-sided CHF. Pleural effusions may be unilateral or bilateral and can cause symptoms such as dyspnea, chest discomfort, and diminished breath sounds on auscultation.
Diagnostic Evaluation of Right-Sided Congestive Heart Failure
The diagnosis of right-sided congestive heart failure is established through a combination of clinical assessment, imaging studies, and laboratory tests. Key investigations may include:
Echocardiography: Transthoracic echocardiography allows for the assessment of right ventricular size and function, estimation of pulmonary artery pressures, detection of valvular abnormalities, and evaluation of pericardial effusions.
Chest X-ray: Chest radiography may reveal cardiomegaly, pulmonary congestion, pleural effusions, and signs of underlying lung disease.
Electrocardiography (ECG): An ECG may demonstrate signs of right ventricular hypertrophy, right atrial enlargement, or conduction abnormalities suggestive of right-sided CHF.
Laboratory Tests: Blood tests may be performed to evaluate for markers of cardiac injury (e.g., troponin), renal function (e.g., creatinine), electrolyte abnormalities, and liver function (e.g., liver enzymes, bilirubin).
What Are The Main,Medications for The Treatment of Right-Sided Congestive Heart Failure?
Diuretics: Diuretic therapy, such as loop diuretics (e.g., furosemide) or thiazide diuretics (e.g., hydrochlorothiazide), is commonly used to promote diuresis and reduce fluid overload in patients with right-sided CHF.
Vasodilators: Pulmonary vasodilators, including phosphodiesterase-5 (PDE-5) inhibitors (e.g., sildenafil) and endothelin receptor antagonists (e.g., bosentan), may be beneficial in patients with pulmonary hypertension and right-sided CHF.
Sodium Restriction: Dietary sodium restriction is recommended to reduce fluid retention and minimize congestion in patients with right-sided CHF. Patients should aim to limit their sodium intake to less than 2 grams per day.
Conclusion
In conclusion, right-sided congestive heart failure is a complex and challenging condition characterized by impaired right ventricular function and venous congestion. Recognition of the signs and symptoms of right-sided CHF is crucial for timely diagnosis and appropriate management. Peripheral edema, ascites, hepatomegaly, jugular venous distension, hepatojugular reflux, and pleural effusions are among the key clinical manifestations observed in patients with right-sided CHF.
Diagnostic evaluation typically involves a combination of clinical assessment, imaging studies, and laboratory tests to confirm the diagnosis and assess disease severity. Treatment strategies focus on alleviating symptoms, improving cardiac function, and optimizing patient outcomes through pharmacotherapy, lifestyle modifications, and close monitoring.
FAQs
Diagnostic Criteria for Congestive Heart Failure:
Clinical Symptoms: Symptoms such as dyspnea (shortness of breath), fatigue, orthopnea (difficulty breathing while lying flat), paroxysmal nocturnal dyspnea (sudden onset of difficulty breathing at night), and peripheral edema (swelling in the legs, ankles, or abdomen) are characteristic of congestive heart failure.
Physical Examination: Findings on physical examination may include elevated jugular venous pressure, displaced apical impulse, third or fourth heart sounds (S3 or S4), crackles in the lungs, hepatomegaly, and peripheral edema.
Imaging Studies: Echocardiography is a key diagnostic tool for evaluating cardiac structure and function in patients with suspected CHF. Echocardiography can assess left ventricular ejection fraction (LVEF), chamber size, wall thickness, valvular function, and the presence of pericardial effusion.
Causes of Heart Failure:
Common causes of heart failure include:
Coronary Artery Disease (CAD): Narrowing or blockage of the coronary arteries can lead to myocardial ischemia and subsequent myocardial infarction (heart attack), resulting in myocardial damage and impaired cardiac function.
Hypertension: Chronic high blood pressure can cause left ventricular hypertrophy and diastolic dysfunction, leading to heart failure with preserved ejection fraction (HFpEF).
Cardiomyopathies: Conditions such as dilated cardiomyopathy, hypertrophic cardiomyopathy, and restrictive cardiomyopathy can directly affect myocardial structure and function, leading to heart failure.
Valvular Heart Disease: Abnormalities of the heart valves, including aortic stenosis, mitral regurgitation, and mitral stenosis, can result in volume overload, pressure overload, or both, ultimately leading to heart failure.
Caring for Heart Failure:
Medication Management: Pharmacotherapy plays a central role in the management of heart failure, with medications such as:
- angiotensin-converting enzyme (ACE) inhibitors,
- angiotensin receptor blockers (ARBs),
- beta-blockers,
- diuretics,
- mineralocorticoid receptor
- antagonists (MRAs),
- sacubitril/valsartan (ARNI) commonly prescribed to optimize cardiac function and alleviate symptoms.