Congestive heart failure (CHF), also known as heart failure, is a chronic condition characterized by the heart’s inability to pump blood efficiently to meet the body’s needs. Diagnosing CHF involves a combination of medical history, physical examination, imaging tests, laboratory studies, and specialized procedures to assess cardiac function, identify underlying causes, and determine the most appropriate treatment plan for individual patients.
Introduction To Congestive Heart Failure
Congestive heart failure (CHF) is a complex clinical syndrome characterized by the heart’s inability to pump blood efficiently to meet the body’s metabolic demands. This results in fluid retention, congestion, and inadequate perfusion of vital organs, leading to a variety of symptoms such as dyspnea (shortness of breath), fatigue, edema (swelling), and exercise intolerance. Diagnosing CHF requires a comprehensive evaluation that incorporates clinical assessment, diagnostic tests, and specialized procedures to assess cardiac structure and function, identify underlying etiologies, and formulate an optimal management plan.
Medical History And Physical Examination
The initial evaluation for suspected congestive heart failure begins with a thorough medical history and physical examination to assess symptoms, risk factors, and potential precipitating factors. Key elements of the medical history include:
Symptoms: Inquire about symptoms such as dyspnea, fatigue, orthopnea (difficulty breathing while lying flat), paroxysmal nocturnal dyspnea (sudden awakening with shortness of breath), edema, and exercise intolerance.
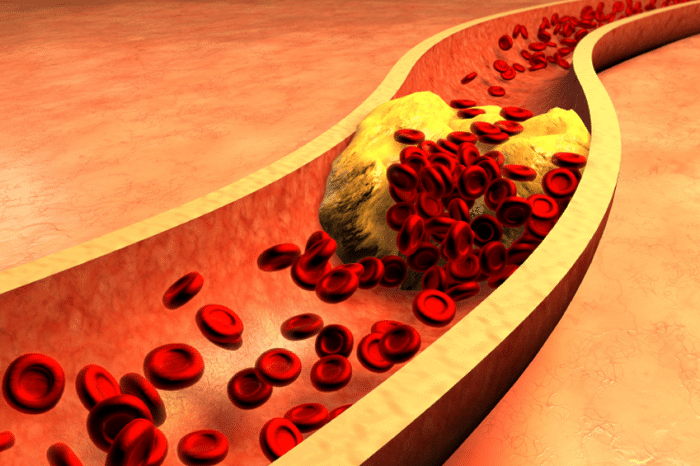
Past medical history: Assess for risk factors and comorbidities such as hypertension, coronary artery disease, diabetes, obesity, valvular heart disease, and prior myocardial infarction.
Medications: Review current medications, including prescription drugs, over-the-counter medications, and supplements, as some medications may exacerbate or precipitate heart failure.
Social history: Inquire about lifestyle factors such as :
- smoking
- alcohol consumption
- dietary habits
- physical activity level
- exposure to environmental toxins or pollutants
Diagnostic Tests for Congestive Heart Failure
The diagnosis of congestive heart failure involves a combination of diagnostic tests and procedures aimed at assessing cardiac structure and function, identifying underlying etiologies, and evaluating the severity of heart failure. Key diagnostic tests for congestive heart failure include:
Electrocardiography (ECG or EKG): Electrocardiography is a non-invasive test that records the heart’s electrical activity and can identify arrhythmias, conduction abnormalities, and signs of cardiac ischemia or hypertrophy.
Echocardiography: Echocardiography is a non-invasive imaging test that uses sound waves to create detailed images of the heart’s structure and function. It can assess cardiac chamber size, wall thickness, ejection fraction, valvular function, and presence of pericardial effusion.
Chest X-ray: Chest X-ray may reveal cardiomegaly (enlarged heart), pulmonary congestion, pleural effusions, and other signs of congestive heart failure such as Kerley B lines or Bat’s wing pattern.
Laboratory studies: Laboratory tests such as complete blood count (CBC), electrolyte panel, renal function tests, liver function tests, thyroid function tests, and brain natriuretic peptide (BNP) or N-terminal pro-B-type natriuretic peptide (NT-proBNP) levels may be ordered to assess for anemia, electrolyte imbalances, renal dysfunction, liver dysfunction, thyroid dysfunction, and myocardial stress.
Invasive Hemodynamic Assessment
In select cases, invasive hemodynamic assessment may be indicated to evaluate cardiac function, assess filling pressures, and guide therapeutic interventions in patients with refractory heart failure or complex hemodynamic abnormalities. Invasive hemodynamic monitoring techniques include:
Right heart catheterization: Right heart catheterization involves the placement of a catheter into the right side of the heart and pulmonary artery to measure pressures and assess cardiac output, pulmonary vascular resistance, and intracardiac filling pressures.
Swan-Ganz catheterization: Swan-Ganz catheterization is a specialized form of right heart catheterization that allows for the measurement of pulmonary artery pressures, pulmonary capillary wedge pressure (PCWP), and mixed venous oxygen saturation (SvO2) to assess cardiac function and hemodynamic status.
Conclusion
In conclusion, diagnosing congestive heart failure requires a comprehensive evaluation that incorporates medical history, physical examination, diagnostic tests, and specialized procedures to assess cardiac structure and function, identify underlying etiologies, and determine the most appropriate treatment plan for individual patients. Electrocardiography, echocardiography, chest X-ray, laboratory studies, advanced imaging modalities, and invasive hemodynamic assessment are essential components of the diagnostic workup for congestive heart failure, providing valuable information to guide clinical decision-making and optimize patient outcomes.
Early and accurate diagnosis of congestive heart failure is crucial for initiating timely interventions, reducing morbidity and mortality, and improving quality of life for patients living with this chronic cardiovascular condition.
FAQs
How is heart failure diagnosed?
Physical Examination: The healthcare provider will perform a physical examination to assess vital signs, heart sounds, lung sounds, presence of edema (swelling), and signs of fluid retention. They may also look for specific physical findings such as elevated jugular venous pressure, hepatojugular reflux, and pulsatile liver.
Electrocardiography (ECG or EKG): This non-invasive test records the heart’s electrical activity and can identify arrhythmias, conduction abnormalities, and signs of cardiac ischemia or hypertrophy.
Echocardiography: Also known as an echo, this imaging test uses sound waves to create detailed images of the heart’s structure and function. It can assess cardiac chamber size, wall thickness, ejection fraction, valvular function, and presence of pericardial effusion.
Chest X-ray: A chest X-ray may reveal signs of congestive heart failure such as cardiomegaly (enlarged heart), pulmonary congestion, pleural effusions, and Kerley B lines.
What are the symptoms of heart failure?
- Shortness of breath (dyspnea), especially with exertion or when lying flat.
- Fatigue and weakness.
- Swelling in the legs, ankles, feet, or abdomen (edema).
- Rapid or irregular heartbeat.
- Persistent cough or wheezing.
- Increased need to urinate at night (nocturia).
- Sudden weight gain due to fluid retention.
How long can one live with first stage heart failure?
Regarding life expectancy with first-stage heart failure, also known as Stage A heart failure, individuals are at risk of developing heart failure but do not yet have symptoms or structural heart abnormalities. With appropriate management, including lifestyle modifications, medication therapy, and regular medical follow-up, individuals with Stage A heart failure can often delay or prevent disease progression and live relatively normal lives.
However, without proper management, Stage A heart failure can progress to more advanced stages associated with increased morbidity and mortality. Therefore, early detection and intervention are crucial for optimizing outcomes and improving quality of life for individuals at risk of heart failure.