Myocarditis, an inflammatory condition of the heart muscle, has garnered increased attention in recent times, particularly in association with mRNA vaccines. As the world grapples with the COVID-19 pandemic, vaccines developed using mRNA technology have emerged as a crucial tool in combating the spread of the virus. However, reports of myocarditis occurring after mRNA vaccination have raised concerns and sparked inquiries into the underlying mechanisms. In this article, we delve into the intricacies of myocarditis and explore why mRNA vaccines may trigger this adverse reaction.
The Basics of Myocarditis
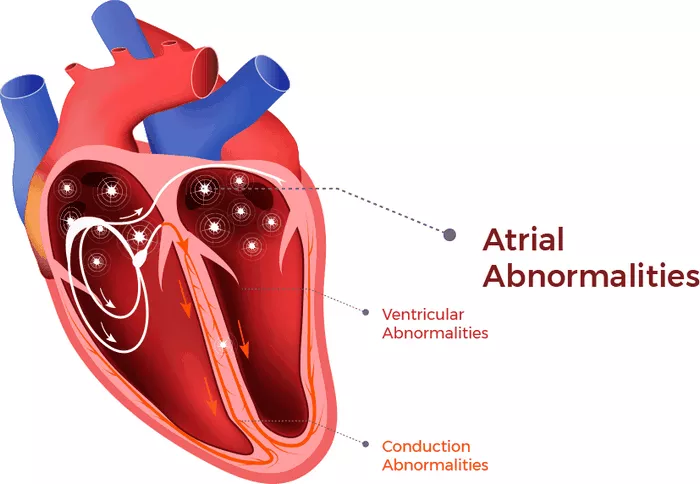
Before delving into the relationship between mRNA and myocarditis, it is essential to understand the fundamentals of this cardiac condition. Myocarditis refers to inflammation of the myocardium, the muscular layer of the heart. It can be caused by various factors, including viral infections, autoimmune diseases, and adverse drug reactions. Myocarditis can manifest acutely or chronically and may lead to a range of symptoms, from mild chest discomfort to severe heart failure and arrhythmias.
The Rise of mRNA Vaccines
mRNA vaccines represent a groundbreaking advancement in vaccine technology. Unlike traditional vaccines, which use weakened or inactivated viruses to stimulate an immune response, mRNA vaccines deliver genetic instructions to cells, instructing them to produce a protein that triggers an immune response against a specific pathogen—in this case, the spike protein of the SARS-CoV-2 virus.
Understanding Myocarditis Post-mRNA Vaccination
While mRNA vaccines have demonstrated remarkable efficacy in preventing COVID-19 and its complications, reports of myocarditis following vaccination have raised concerns among healthcare professionals and the public alike. Myocarditis cases predominantly affect younger individuals, particularly males, and often occur within days to weeks after vaccination. The symptoms typically include chest pain, shortness of breath, and palpitations, mirroring those of myocarditis from other causes.
What Is The Relationship Between mRNA Vaccination And Myocarditis?
The precise mechanisms underlying mRNA vaccine-associated myocarditis remain under investigation. Several hypotheses have been proposed to explain the link between mRNA vaccination and myocarditis:
Immune Response to Spike Protein:
One theory suggests that the immune response triggered by mRNA vaccines, specifically targeting the spike protein of the SARS-CoV-2 virus, may inadvertently lead to inflammation in cardiac tissues. The spike protein shares structural similarities with proteins expressed in cardiac muscle cells, potentially eliciting an immune response that targets both viral and cardiac proteins.
Adjuvants And Vaccine Components:
Another possibility is that certain components of the mRNA vaccine formulation, such as lipid nanoparticles or adjuvants, could trigger an exaggerated immune response in susceptible individuals. Adjuvants are substances added to vaccines to enhance the immune response, but they may also increase the risk of adverse reactions in some individuals.
Individual Susceptibility:
It is widely recognized that individual factors, including genetic predisposition and underlying health conditions, can influence the risk of developing myocarditis. Some individuals may have preexisting immune dysregulation or genetic variants that predispose them to inflammatory reactions following vaccination.
Viral Coinfection:
In some cases, individuals may be coincidentally infected with a viral pathogen around the time of vaccination, leading to synergistic effects that exacerbate immune-mediated inflammation in the heart.
Clinical Implications and Risk-Benefit Analysis
Future Directions And Research
As the scientific community continues to investigate the relationship between mRNA vaccines and myocarditis, ongoing research endeavors aim to elucidate the underlying mechanisms, identify risk factors, and develop strategies for risk mitigation and management. Longitudinal studies tracking the incidence of myocarditis post-vaccination and assessing its long-term outcomes will provide valuable insights into the safety profile of mRNA vaccines.
Conclusion
Myocarditis remains a complex and multifaceted condition, and its association with mRNA vaccination underscores the importance of ongoing vigilance and research in vaccine safety. While the exact mechanisms linking mRNA vaccines to myocarditis are not yet fully understood, it is crucial to balance the benefits of vaccial risks of adverse reactions. By advancing our understanding of myocarditis and mRNA vaccine safety, we can optimize public health strategies and ensure the continued development and deployment of safe and effective vaccines.
FAQs
What are the side effects caused by mRNA vaccines?
Side effects of mRNA vaccines, such as those developed by Pfizer-BioNTech and Moderna, are generally mild to moderate and temporary. Common side effects include pain or swelling at the injection site, fatigue, headache, muscle or joint pain, chills, fever, and nausea. These side effects typically resolve within a few days after vaccination. Serious side effects are rare but can include severe allergic reactions (anaphylaxis).
What should we pay attention to in myocarditis?
In myocarditis, it’s crucial to pay attention to symptoms such as :
- chest pain
- shortness of breath
- fatigue
- rapid
- irregular heartbeat
- swelling in the legs
- ankles
- feet
These symptoms can indicate inflammation of the heart muscle, which requires medical attention. Additionally, symptoms of myocarditis can sometimes mimic those of a heart attack, so it’s essential to seek prompt medical evaluation if you experience any concerning symptoms.
What medicine should I take for myocarditis?
The treatment for myocarditis depends on the severity of the condition and its underlying cause. In some cases, supportive care, such as rest and over-the-counter pain relievers, may be sufficient to manage mild symptoms.
However, if symptoms are severe or complications such as heart failure or arrhythmias develop, more aggressive treatment may be necessary. This can include medications to reduce inflammation (such as nonsteroidal anti-inflammatory drugs or corticosteroids), medications to manage symptoms (such as diuretics or beta-blockers), and in some cases, interventions such as implantable devices or procedures to treat complications.