Cardiac arrest and heart failure are two distinct yet interrelated cardiac conditions that can have serious implications for a person’s health and well-being. While both involve the heart, they differ significantly in their causes, symptoms, and outcomes.
Cardiac Arrest: A Sudden Stoppage of Heart Function
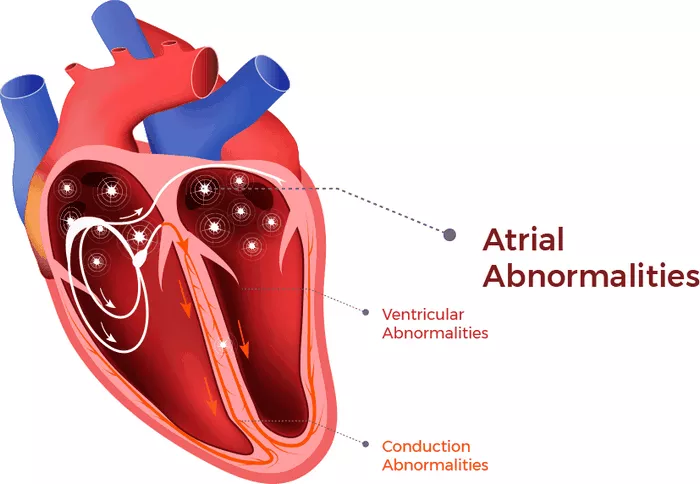
Cardiac arrest is a medical emergency characterized by the sudden cessation of heart function, resulting in the loss of blood flow to vital organs. It occurs when the heart’s electrical system malfunctions, leading to abnormal heart rhythms (arrhythmias) that disrupt the heart’s pumping action. Without prompt intervention, cardiac arrest can quickly lead to unconsciousness, cessation of breathing, and death within minutes.
Causes of Cardiac Arrest
Cardiac arrest can occur due to various underlying causes, including:
Ventricular Fibrillation: Ventricular fibrillation is the most common arrhythmia associated with cardiac arrest. It occurs when the heart’s lower chambers (ventricles) quiver rapidly and irregularly, preventing effective blood pumping.
Ventricular Tachycardia: Ventricular tachycardia is a rapid heartbeat originating from the ventricles, which can degenerate into ventricular fibrillation if left untreated.
Bradycardia: Bradycardia refers to an abnormally slow heart rate, which can lead to inadequate blood flow and cardiac arrest if severe.
Myocardial Infarction (Heart Attack): A heart attack occurs when blood flow to a part of the heart is blocked, leading to damage or death of the heart muscle. In some cases, a heart attack can trigger cardiac arrest due to the disruption of the heart’s electrical system.
Electrolyte Imbalances: Abnormal levels of potassium, magnesium, or calcium in the blood can affect the heart’s electrical activity and increase the risk of arrhythmias and cardiac arrest.
Drug Overdose: Certain medications, illicit drugs, or toxins can interfere with the heart’s electrical signals and precipitate cardiac arrest.
Symptoms of Cardiac Arrest
Cardiac arrest often occurs suddenly and without warning, and the affected individual may experience:
- Sudden loss of consciousness
- Absence of pulse or breathing
- Gasping or abnormal breathing (agonal respirations)
- Loss of color (pallor) or cyanosis (bluish discoloration) of the skin
- Treatment of Cardiac Arrest
Cardiac arrest is a medical emergency that requires immediate intervention to restore normal heart function and circulation. Treatment may include:
Cardiopulmonary Resuscitation (CPR): CPR involves chest compressions and rescue breaths to manually circulate oxygenated blood to vital organs until advanced life support measures can be initiated.
Defibrillation: Defibrillation delivers an electrical shock to the heart to restore normal heart rhythm, particularly in cases of ventricular fibrillation or pulseless ventricular tachycardia.
Advanced Cardiac Life Support (ACLS): ACLS protocols involve advanced interventions such as medications (e.g., epinephrine, amiodarone), advanced airway management, and post-resuscitation care in a hospital setting.
Identifying and Treating Underlying Causes: Once the patient is stabilized, efforts focus on identifying and treating the underlying cause of cardiac arrest to prevent recurrence.
Heart Failure: A Chronic Condition of Impaired Heart Function
Heart failure is a chronic medical condition characterized by the heart’s inability to pump blood effectively to meet the body’s demands. It develops over time as a result of various underlying cardiac or systemic conditions that damage the heart muscle or impair its function. Heart failure can affect the heart’s ability to fill with blood (diastolic dysfunction) or eject blood during contraction (systolic dysfunction), leading to a cascade of symptoms and complications.
Causes of Heart Failure
Heart failure can be caused by a variety of factors, including:
Coronary Artery Disease: Narrowing or blockage of the coronary arteries reduces blood flow to the heart muscle, leading to myocardial ischemia and damage. Chronic ischemic heart disease can ultimately result in heart failure.
Hypertension: Persistent high blood pressure increases the workload on the heart, causing the heart muscle to thicken and stiffen over time (left ventricular hypertrophy). This can impair cardiac function and contribute to heart failure.
Cardiomyopathy: Cardiomyopathy refers to diseases of the heart muscle that weaken the heart’s pumping ability. Types of cardiomyopathy include dilated cardiomyopathy, hypertrophic cardiomyopathy, and restrictive cardiomyopathy.
Valvular Heart Disease: Malfunctioning heart valves (e.g., aortic stenosis, mitral regurgitation) can disrupt normal blood flow through the heart chambers, leading to volume overload, pressure overload, or both, and ultimately causing heart failure.
Myocarditis: Myocarditis is inflammation of the heart muscle, often due to viral infections or autoimmune reactions. Severe myocarditis can impair cardiac function and contribute to heart failure.
Other Conditions: Heart failure can also result from congenital heart defects, arrhythmias, diabetes, obesity, thyroid disorders, and certain medications or toxins.
Symptoms of Heart Failure
Heart failure can present with a variety of symptoms, which may include:
- Shortness of breath (dyspnea), especially during exertion or when lying flat
- Fatigue and weakness
- Swelling in the legs, ankles, or abdomen (edema)
- Persistent coughing or wheezing
- Rapid or irregular heartbeat (palpitations)
- Reduced exercise tolerance
- Sudden weight gain due to fluid retention
- Classification of Heart Failure
Heart failure is typically classified based on the severity of symptoms and the degree of impairment of cardiac function.
The New York Heart Association (NYHA) functional classification system categorizes heart failure into four classes:
Class I (Mild): No limitation of physical activity; ordinary physical activity does not cause symptoms.
Class II (Mild to Moderate): Slight limitation of physical activity; comfortable at rest, but ordinary physical activity results in symptoms.
Class III (Moderate to Severe): Marked limitation of physical activity; comfortable at rest, but less than ordinary activity causes symptoms.
Class IV (Severe): Unable to carry out any physical activity without discomfort; symptoms present at rest and worsen with any physical activity.
Conclusion
While cardiac arrest and heart failure both involve the heart, they represent distinct clinical entities with different pathophysiological mechanisms, presentations, and management approaches. Cardiac arrest is a sudden, life-threatening event characterized by the abrupt cessation of heart function and circulation, requiring immediate intervention to restore cardiac rhythm and perfusion.
In contrast, heart failure is a chronic condition marked by the heart’s inability to pump blood efficiently, leading to symptoms such as fatigue, dyspnea, and fluid retention. Management of cardiac arrest focuses on prompt recognition, bystander CPR, defibrillation, and advanced life support measures, while heart failure management aims to alleviate symptoms, slow disease progression, and improve quality of life through medications, lifestyle modifications, and, in some cases
FAQs
How long can an elderly person live with heart failure?
The prognosis for elderly individuals with heart failure depends on various factors, including the severity of the condition, the presence of comorbidities, the effectiveness of treatment, and the individual’s overall health and functional status. While heart failure is a serious and chronic condition, many elderly individuals can live for several years with proper management and care.
It’s important to note that heart failure is a progressive condition that typically worsens over time, particularly if left untreated or poorly managed. However, with advances in medical treatment, including medications, lifestyle modifications, and devices such as implantable cardioverter-defibrillators (ICDs) and cardiac resynchronization therapy (CRT), many elderly individuals with heart failure can achieve symptom relief, improve their quality of life, and prolong survival.
Can I exercise if I have heart failure?
Heart failure makes the heart weak. Patients who are taking medication or after surgery can start taking care of their health by starting with light exercise. Perform regular rehabilitation exercises under the guidance of a physical therapist.
Rehabilitation exercises can help strengthen muscles and bones, relieve stress, improve breathing and sleep, and enhance physical health. Patients can also get back on track and live an active life as soon as possible.
If someone experiences symptoms of cardiac arrest or witnesses someone collapsing unexpectedly, it’s essential to call emergency services (such as 911 in the United States) and initiate cardiopulmonary resuscitation (CPR) until help arrives.
Can heart failure be cured?
Heart failure is a chronic and progressive condition characterized by the heart’s inability to pump blood effectively to meet the body’s demands. While heart failure cannot typically be cured in the traditional sense, it can be managed effectively with appropriate treatment and lifestyle modifications.
Lifestyle Modifications: Lifestyle changes, such as following a heart-healthy diet low in sodium, exercising regularly, maintaining a healthy weight, limiting alcohol intake, quitting smoking, and managing stress, are essential for managing heart failure and improving outcomes.
Device Therapy: Implantable devices, such as implantable cardioverter-defibrillators (ICDs) and cardiac resynchronization therapy (CRT) devices, may be recommended for certain individuals with heart failure to help regulate heart rhythm and improve cardiac function.
While heart failure may not be curable in the traditional sense, many individuals with the condition can lead fulfilling lives with proper management and care. It’s essential for individuals with heart failure to work closely with their healthcare