Among the various types of arrhythmias, ventricular fibrillation stands out as one of the most dangerous and potentially life-threatening. This irregular heart rhythm disrupts the heart’s ability to pump blood effectively, leading to a rapid and chaotic heartbeat. In this comprehensive article, we will delve into what ventricular fibrillation is, its causes, symptoms, diagnosis, and treatment options.
The Most Dangerous Type of Arrhythmia(Ventricular Fibrillation)
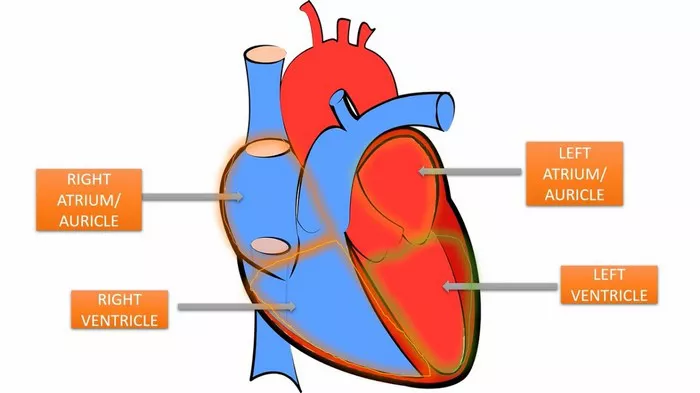
Ventricular fibrillation (VF) is a type of arrhythmia characterized by rapid and chaotic electrical activity in the ventricles, the lower chambers of the heart. During ventricular fibrillation, the heart’s electrical signals become disorganized, causing the ventricles to quiver ineffectively instead of contracting and pumping blood. As a result, blood flow to vital organs is severely compromised, leading to a sudden loss of consciousness and, if not promptly treated, death.
Causes of Ventricular Fibrillation
Ventricular fibrillation can occur spontaneously or be triggered by various underlying factors. Some common causes and contributing factors include:
Coronary Artery Disease (CAD): The most common cause of ventricular fibrillation is coronary artery disease, which results in the narrowing or blockage of the coronary arteries supplying blood to the heart muscle. When blood flow to the heart is significantly reduced or obstructed, it can lead to myocardial ischemia (lack of oxygen to the heart muscle) and subsequent ventricular fibrillation.
Previous Heart Attack: Individuals who have experienced a previous heart attack are at increased risk of developing ventricular fibrillation, especially if the heart muscle has been damaged or scarred as a result of the infarction. Scar tissue in the heart can disrupt the normal electrical conduction system, predisposing to arrhythmias such as ventricular fibrillation.
Cardiomyopathy: Certain types of cardiomyopathy, such as hypertrophic cardiomyopathy or dilated cardiomyopathy, can weaken the heart muscle and disrupt its electrical activity, increasing the risk of ventricular fibrillation.
Electrolyte Imbalances: Abnormal levels of electrolytes such as potassium, sodium, or calcium in the blood can affect the heart’s electrical conduction system and trigger ventricular fibrillation.
Drug Toxicity: Certain medications, recreational drugs, or toxins can interfere with normal cardiac function and predispose individuals to ventricular fibrillation. These may include antiarrhythmic drugs, certain antibiotics, or illicit drugs such as cocaine.
Symptoms of Ventricular Fibrillation
Unlike other types of arrhythmias, ventricular fibrillation often presents with sudden and severe symptoms, as it can quickly lead to cardiac arrest and loss of consciousness.
Some common symptoms of ventricular fibrillation may include:
Loss of Consciousness: Sudden loss of consciousness is a hallmark symptom of ventricular fibrillation. This occurs when the brain is deprived of oxygen due to inadequate blood flow resulting from the chaotic heart rhythm.
No Pulse: During ventricular fibrillation, the heart’s ineffective quivering prevents it from effectively pumping blood, resulting in the absence of a palpable pulse.
No Breathing: Ventricular fibrillation can also cause a sudden cessation of breathing as a result of the inadequate blood flow to the lungs and subsequent lack of oxygen delivery to the brain.
Diagnosis of Ventricular Fibrillation
Diagnosing ventricular fibrillation often occurs in emergency settings when an individual presents with sudden cardiac arrest.These tests may include:
Electrocardiogram (ECG or EKG): An ECG is a standard diagnostic test used to measure the heart’s electrical activity. In ventricular fibrillation, the ECG will show a chaotic and irregular pattern indicative of rapid and disorganized electrical signals in the ventricles.
Blood Tests: Blood tests may be performed to assess levels of electrolytes, cardiac enzymes, and other markers of heart damage, which can help identify underlying causes of ventricular fibrillation such as myocardial infarction or electrolyte imbalances.
Echocardiogram: An echocardiogram uses sound waves to create images of the heart’s structure and function. This test can help evaluate the heart’s pumping function, identify structural abnormalities, and assess for underlying heart conditions that may predispose to ventricular fibrillation.
Cardiac Monitoring: Continuous cardiac monitoring, such as telemetry or Holter monitoring, may be used to assess the heart’s rhythm over an extended period and capture any episodes of ventricular fibrillation that occur outside of the hospital setting.
Conclusion
Ventricular fibrillation is a life-threatening arrhythmia characterized by rapid and chaotic electrical activity in the heart’s ventricles. Without prompt intervention, ventricular fibrillation can quickly lead to cardiac arrest and death. Recognizing the symptoms of ventricular fibrillation and seeking immediate medical attention is crucial for improving outcomes and reducing mortality rates associated with this dangerous arrhythmia.
By implementing advanced cardiac care techniques such as defibrillation, CPR, antiarrhythmic medications, and implantable devices, healthcare providers can effectively manage ventricular fibrillation and improve survival rates for individuals at risk. Early recognition, timely intervention, and ongoing management are essential for optimizing outcomes and reducing the devastating impact of ventricular fibrillation on individuals and communities.
FAQs
How to treat ventricular fibrillation?
Defibrillation: Defibrillation is the most critical intervention for terminating ventricular fibrillation and restoring normal heart rhythm. It involves delivering an electric shock to the chest using a defibrillator device, which temporarily interrupts the chaotic electrical activity in the heart and allows the normal pacemaker cells to regain control.
Cardiopulmonary Resuscitation (CPR): CPR may be initiated immediately to maintain blood flow to vital organs until defibrillation can be performed. CPR involves chest compressions to manually pump blood through the body and artificial ventilation to deliver oxygen to the lungs.
Antiarrhythmic Medications: After successful defibrillation, antiarrhythmic medications such as amiodarone, lidocaine, or procainamide may be administered to stabilize the heart’s electrical activity and prevent recurrence of ventricular fibrillation.
Implantable Cardioverter-Defibrillator (ICD): For individuals at high risk of recurrent ventricular fibrillation, implantable cardioverter-defibrillators (ICDs) may be recommended. An ICD is a small device implanted under the skin that continuously monitors the heart’s rhythm and delivers electrical shocks when it detects ventricular fibrillation or other life-threatening arrhythmias.
Coronary Revascularization: If ventricular fibrillation is caused by underlying coronary artery disease, interventions such as percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) may be necessary to restore blood flow to the heart muscle and reduce the risk of recurrent arrhythmias.
Is an irregular heartbeat dangerous?
Whether an irregular heartbeat is dangerous depends on the specific type of arrhythmia and its underlying causes. Some irregular heart rhythms, such as premature atrial or ventricular contractions, are relatively common and often benign, especially in individuals without underlying heart disease. However, other arrhythmias, such as ventricular fibrillation or sustained ventricular tachycardia, can be life-threatening and require immediate medical attention.
If you have been diagnosed with an irregular heartbeat, it’s essential to work closely with your healthcare provider to determine the type and severity of the arrhythmia, as well as any underlying heart conditions that may be contributing to it. Your healthcare provider can recommend appropriate treatment and lifestyle modifications to help manage the arrhythmia and reduce the risk of complications.
Can I run if I have an irregular heartbeat?
As for running with an irregular heartbeat, it depends on your individual circumstances and the recommendations of your healthcare provider. In many cases, individuals with well-controlled arrhythmias may be able to engage in regular exercise, including running, as part of a healthy lifestyle. However, it’s essential to consult with your healthcare provider before starting any new exercise program, especially if you have a known heart condition or arrhythmia.
Your healthcare provider may recommend certain precautions or modifications to your exercise routine based on your specific situation, such as monitoring your heart rate during exercise, avoiding high-intensity activities, or adjusting your medications as needed.