Atrial fibrillation (AFib) is a common cardiac arrhythmia characterized by irregular and often rapid heartbeats. It affects millions of people worldwide and is associated with various cardiovascular and systemic symptoms. One question that frequently arises among individuals with AFib or those at risk of developing it is whether AFib can cause shortness of breath. This article delves into the complexities of this topic, examining the mechanisms, clinical manifestations, and management strategies related to AFib and respiratory symptoms.
Understanding Atrial Fibrillation
Before exploring the link between AFib and shortness of breath, it’s essential to understand the basics of this cardiac arrhythmia. In a normal heart rhythm, the atria (upper chambers) contract synchronously, followed by the ventricles (lower chambers), resulting in an efficient pumping of blood throughout the body. However, in AFib, the electrical signals that coordinate heartbeats become chaotic, leading to irregular and rapid heartbeats.
Common symptoms of AFib include palpitations, chest discomfort, fatigue, and dizziness. The irregular heart rhythm can also predispose individuals to other cardiovascular complications, such as stroke and heart failure.
Mechanisms of Shortness of Breath in AFib
Shortness of breath, medically known as dyspnea, can occur in individuals with AFib due to several interconnected mechanisms:
Decreased Cardiac Output: In AFib, the irregular heart rhythm may compromise the heart’s ability to pump blood effectively. This reduced cardiac output can lead to inadequate oxygen delivery to tissues, including the lungs, resulting in dyspnea.
Heart Failure: AFib is a common comorbidity in heart failure patients. Heart failure occurs when the heart is unable to pump blood efficiently, leading to fluid buildup in the lungs (pulmonary congestion) and subsequent shortness of breath.
Atrial Stretch and Remodeling: Chronic AFib can cause structural changes in the atria, including dilation and fibrosis. These changes may affect the atrial function and contribute to fluid retention and pulmonary congestion, exacerbating respiratory symptoms.
Underlying Lung Conditions: Some individuals with AFib may have concurrent lung diseases, such as chronic obstructive pulmonary disease (COPD) or pulmonary hypertension, which can independently cause dyspnea. AFib may exacerbate these conditions or be exacerbated by them.
Clinical Manifestations
The relationship between AFib and shortness of breath is not always straightforward. Some individuals with AFib may experience significant dyspnea, while others may have minimal respiratory symptoms. The severity and frequency of dyspnea can vary based on several factors, including:
Underlying Cardiovascular Health: The presence of other cardiovascular conditions, such as heart failure or coronary artery disease, can influence the impact of AFib on respiratory symptoms.
AFib Type: Paroxysmal AFib (intermittent episodes) may result in transient dyspnea during arrhythmia episodes, whereas persistent or permanent AFib may contribute to chronic dyspnea.
Rate and Rhythm Control: The management approach for AFib, whether focused on controlling heart rate or restoring normal sinus rhythm, can affect symptoms such as dyspnea.
Individual Variability: Each person’s response to AFib and its associated symptoms, including dyspnea, can vary based on genetic, physiological, and lifestyle factors.
Diagnostic Evaluation
When evaluating a patient with AFib and shortness of breath, healthcare providers typically conduct a thorough assessment to determine the underlying causes and appropriate management. Diagnostic steps may include:
Medical History and Physical Examination: Gathering information about the patient’s cardiovascular health, symptoms, and risk factors can provide valuable insights.
Electrocardiogram (ECG): ECG is the primary tool for diagnosing AFib and assessing its characteristics, including heart rate and rhythm.
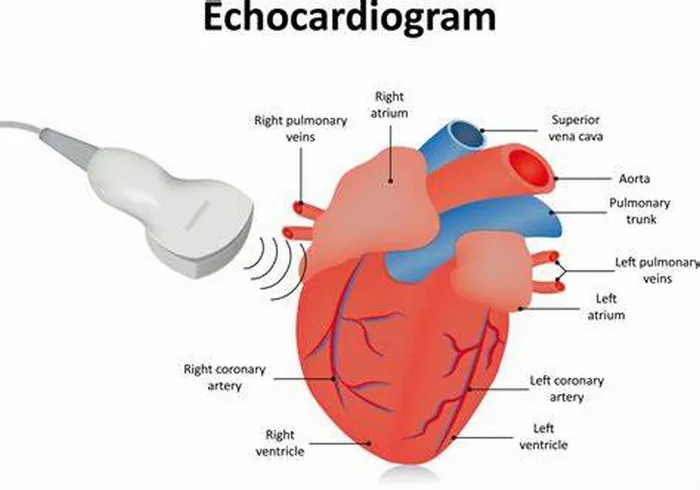
Echocardiogram: This imaging test evaluates the structure and function of the heart, helping identify conditions such as heart failure or valvular abnormalities.
Pulmonary Function Tests: These tests assess lung function and can identify underlying lung diseases contributing to dyspnea.
Cardiac Biomarkers: Blood tests may be performed to evaluate cardiac function and detect markers of heart failure or myocardial injury.
Management Strategies
The management of AFib-related dyspnea focuses on addressing underlying causes, optimizing heart function, and improving quality of life. Key strategies include:
AFib Management: Depending on the type and severity of AFib, treatment approaches may include rate control (medications to regulate heart rate), rhythm control (medications or procedures to restore normal sinus rhythm), and anticoagulation therapy to reduce stroke risk.
Heart Failure Management: For individuals with AFib and heart failure, comprehensive heart failure management strategies, such as medications (e.g., diuretics, ACE inhibitors), lifestyle modifications, and device therapy (e.g., pacemaker, implantable cardioverter-defibrillator), are crucial.
Optimizing Cardiovascular Health: Lifestyle modifications, including regular exercise, a heart-healthy diet, smoking cessation, and stress management, can improve overall cardiovascular health and potentially alleviate dyspnea.
Managing Comorbidities: Addressing concurrent conditions such as lung diseases, hypertension, and diabetes is essential in managing dyspnea and improving overall well-being.
Conclusion
In conclusion, atrial fibrillation can contribute to shortness of breath through multiple mechanisms, including decreased cardiac output, heart failure, atrial remodeling, and underlying lung conditions. The relationship between AFib and dyspnea is complex, influenced by various factors, and may vary among individuals.
A comprehensive evaluation, including medical history, physical examination, and diagnostic tests, is essential in assessing and managing AFib-related dyspnea effectively. Treatment strategies focus on addressing underlying cardiovascular issues, optimizing heart function, and promoting overall cardiovascular health.
While AFib and dyspnea can pose challenges, proactive management, lifestyle modifications, and adherence to treatment plans can lead to improved outcomes and a better quality of life for individuals living with these conditions. Ongoing research and advancements in cardiac care continue to enhance our understanding and management of AFib-related respiratory symptoms, offering hope for a brighter outlook for affected individuals.
FAQs
What is considered a multi-millionaire?
A multi-millionaire typically refers to an individual or household with a net worth exceeding several million dollars. The exact threshold can vary based on context and definitions, but it generally implies having assets, investments, and/or cash holdings valued at multiple millions, such as $2 million, $5 million, $10 million, or more. Being a multi-millionaire signifies significant wealth and financial independence.
What does multimillionnaire mean?
Multimillionnaire is a variation of the term “multi-millionaire” and carries the same meaning. It describes someone who possesses assets, investments, or wealth totaling several million dollars or more. The prefix “multi-” indicates multiple or many, and “millionnaire” refers to a person whose wealth is measured in millions.
How many is a multi-millionaire?
The term “multi-millionaire” implies having a net worth that exceeds one million dollars by a significant margin. The exact number of millions required to be considered a multi-millionaire can vary based on interpretation and context. It typically suggests having assets or wealth valued at several million dollars, such as $2 million, $5 million, $10 million, or more. The term emphasizes substantial wealth beyond a single million-dollar threshold.