Wolff-Parkinson-White (WPW) syndrome is a rare cardiac condition characterized by the presence of an extra electrical pathway in the heart, which can lead to episodes of rapid heart rate (tachycardia). This condition affects individuals of all ages, including infants, children, and adults. It is crucial for medical professionals, patients, and families to understand the nature of this disorder, its clinical manifestations, diagnostic approaches, and the latest treatment options to manage and potentially resolve symptoms effectively.
Historical Background And Epidemiology
Wolff-Parkinson-White syndrome was first described in 1930 by Louis Wolff, John Parkinson, and Paul Dudley White, three prominent cardiologists. The condition is identified as a type of pre-excitation syndrome. In general, WPW syndrome occurs in about 1 to 3 per 1,000 people globally. There is no significant difference in incidence between males and females, and it can occur congenitally or develop later in life.
Pathophysiology of WPW Syndrome
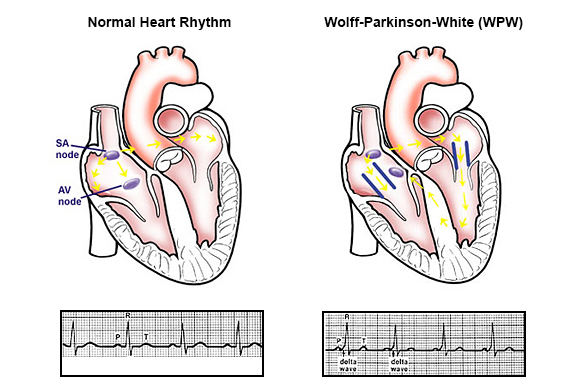
The hallmark of WPW syndrome is an additional electrical pathway known as the accessory pathway or Kent bundle. This pathway bypasses the usual route taken by electrical impulses through the atrioventricular (AV) node. Under normal circumstances, the AV node acts as a gatekeeper, moderating the electrical signals that control heartbeats.
FAHowever, in WPW syndrome, the accessory pathway allows electrical impulses to circumvent the AV node and pre-excite the ventricles, leading to a sequence of rapid heartbeating.
The Mechanism of Tachycardia
In individuals with WPW, tachycardia episodes can be triggered by two main mechanisms:
Orthodromic Reciprocating Tachycardia (ORT): This is the most common form, where the electrical impulse travels down the normal pathway and returns up the accessory pathway, causing a rapid heart rate.
Antidromic Reciprocating Tachycardia (ART): Less common than ORT, in this type, the impulse travels down the accessory pathway and returns via the AV node.
These abnormal electrical circuits disrupt the normal heart rhythm and can lead to palpitations, dizziness, fainting, and even sudden cardiac death if not properly managed.
Clinical Manifestations
Symptoms of WPW syndrome can vary significantly among individuals. Some may remain asymptomatic and unaware of their condition until it is incidentally discovered during an electrocardiogram (ECG) for another reason. Common symptoms include:
- Sudden episodes of rapid heart rate.
- Palpitations or the feeling of fluttering in the chest.
- Dizziness or light-headedness.
- Dyspnea (shortness of breath).
- Syncope (fainting) or near-fainting spells.
In severe cases, particularly when associated with atrial fibrillation, WPW can lead to more significant complications such as congestive heart failure or sudden cardiac arrest.
Diagnosis of WPW Syndrome
The diagnosis of WPW syndrome is primarily based on the findings from an electrocardiogram (ECG). Key features on an ECG indicative of WPW syndrome include:
- A short PR interval less than 120 milliseconds.
- A broad QRS complex greater than 100 milliseconds.
- A delta wave, which is a slurred upstroke in the QRS complex that results from the early excitation of the ventricles due to the presence of the accessory pathway.
Additional diagnostic tests may include:
Holter Monitoring: A continuous ECG recording over 24 to 48 hours to capture transient episodes of tachycardia.
Exercise Stress Testing: To observe the heart’s activity under stress and detect any abnormalities that may not be present at rest.
Electrophysiological Study (EPS): An invasive test performed to pinpoint the exact location of the accessory pathway and to determine the best treatment approach.
Treatment Options
Treatment for WPW syndrome varies based on the severity of symptoms and the risk of more serious arrhythmias. Options include:
Medications: Antiarrhythmic drugs may be used to control episodes of tachycardia. Commonly used medications include beta-blockers, calcium channel blockers, and in some cases, more specific antiarrhythmics like flecainide or propafenone.
Catheter Ablation: This is often the treatment of choice, especially for symptomatic WPW. It involves threading a catheter through the veins into the heart and using radiofrequency energy to destroy the abnormal electrical pathway. This procedure has a high success rate and usually results in a permanent cure of the condition.
Surgery: In rare cases where catheter ablation is not successful or not possible, open-heart surgery might be considered to physically cut the accessory pathway.
Prevention And Prognosis
There is no known prevention for WPW syndrome since it is often congenital. However, with proper management, the prognosis is generally excellent. Most people who undergo successful catheter ablation recover completely and are able to return to normal activities without significant restrictions.
Conclusion
Wolff-Parkinson-White syndrome, while potentially life-threatening, is generally treatable with modern medical approaches. Understanding the pathophysiology, recognizing the clinical manifestations, and applying the correct diagnostic and therapeutic strategies can lead to excellent outcomes for patients. Ongoing research and technological advances continue to improve the diagnosis and treatment of this intriguing cardiac anomaly, offering hope and a better quality of life for those affected.
By fostering awareness and education on WPW syndrome among healthcare providers and patients, it is possible to effectively manage this condition and prevent its most serious complications, thereby ensuring those affected can lead full and active lives.
FAQs
What Causes WPW?
WPW syndrome is present at birth (congenital). The exact cause of WPW syndrome is not well understood, but it involves the presence of an additional electrical pathway between the atria and the ventricles, known as the accessory pathway. This pathway bypasses the usual route, which can cause the electrical signal to travel around the heart too quickly. This results in episodes of tachycardia.
Most cases of WPW syndrome are sporadic, meaning they occur randomly. However, a small percentage of cases appear to have a genetic component, as they run in families.
What Should I Avoid If I Have WPW?
If you have WPW syndrome, certain things should be avoided to help manage the condition and reduce the risk of complications like episodes of rapid heart rate:
Stimulants: Avoid caffeine, alcohol, and smoking, as these can trigger heart rhythm problems.
Certain Medications: Some over-the-counter medications like pseudoephedrine, found in cold medications, can exacerbate symptoms. Always consult with a healthcare provider before taking new medications.
Stress: High stress can trigger tachycardia, so stress management techniques like yoga, meditation, and regular physical activity (as advised by a doctor) can be beneficial.
Excessive Exercise: While regular physical activity is important, extremely vigorous exercise might trigger rapid heart rates. Consult with a cardiologist to determine the appropriate level of exercise.
It’s important to have regular follow-ups with a healthcare provider who can provide personalized advice on what to avoid.
What is the Life Expectancy of a Person with Wolff-Parkinson-White Syndrome?
The life expectancy of a person with WPW syndrome is generally normal, especially with effective management and treatment. The prognosis is excellent for those who receive proper treatment, which may include medications to control episodes of tachycardia or procedures like catheter ablation. Catheter ablation is highly successful and can potentially cure WPW syndrome by destroying the abnormal electrical pathway.
While WPW syndrome can be associated with certain risks like sudden cardiac arrest, these are rare, particularly if the syndrome is diagnosed and treated appropriately. Continuous monitoring and regular consultations with a cardiologist are crucial to effectively manage the condition and maintain a healthy lifestyle.