Supraventricular Tachycardia (SVT) is a common heart rhythm disorder characterized by a rapid heart rate originating from the upper chambers of the heart. Episodes of SVT can be unsettling and disruptive to daily life, prompting individuals to seek a deeper understanding of what triggers these episodes. In this comprehensive guide, we delve into the various factors that can precipitate an SVT episode, shedding light on the intricate interplay of physiological, environmental, and lifestyle elements.
Physiological Triggers
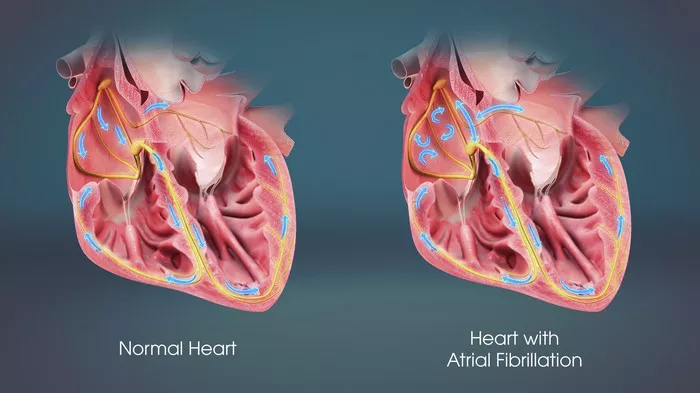
Electrical Pathway Abnormalities: SVT often arises due to abnormalities in the electrical pathways of the heart. Specific conditions such as Wolff-Parkinson-White (WPW) syndrome, where an extra electrical pathway exists, can predispose individuals to SVT episodes.
Hormonal Influences: Fluctuations in hormonal levels, particularly adrenaline and thyroid hormones, can trigger SVT in susceptible individuals. Hormonal changes during pregnancy, menopause, or thyroid disorders may contribute to the onset of episodes.
Heart Structural Anomalies: Structural abnormalities in the heart, such as congenital defects or scarring from previous cardiac events, can create conditions conducive to SVT initiation. Understanding these structural nuances is crucial in managing and preventing episodes.
Autonomic Nervous System Dysfunction: Dysregulation of the autonomic nervous system, responsible for controlling heart rate and rhythm, can lead to erratic heart rate patterns, including SVT. Factors like stress, anxiety, and autonomic neuropathy can influence SVT occurrence.
Environmental Triggers
Stimulant Consumption: Consumption of stimulants such as caffeine, nicotine, and certain medications (e.g., decongestants, bronchodilators) can trigger SVT episodes by increasing heart rate and altering electrical conduction in the heart.
Alcohol and Substance Use: Excessive alcohol intake and recreational drug use have been linked to SVT initiation. The impact of these substances on heart function and rhythm underscores the importance of moderation and awareness.
Temperature Extremes: Exposure to extreme temperatures, whether hot or cold, can provoke SVT episodes in susceptible individuals. Temperature-related stress on the cardiovascular system can disrupt normal heart rhythm.
Environmental Stressors: High-stress environments, exposure to loud noises, and emotional upheavals can act as triggers for SVT. Managing stress and cultivating relaxation techniques are integral to SVT management strategies.
Lifestyle Triggers
Physical Exertion: Intense physical activity or sudden exertion can prompt SVT episodes, especially in individuals with underlying cardiac conditions. Balancing exercise intensity and monitoring heart rate during workouts is essential for SVT management.
Dietary Factors: Certain foods and beverages, such as spicy foods, heavy meals, and high-sugar items, can contribute to SVT triggers. Understanding individual dietary sensitivities and making mindful choices can mitigate risk.
Sleep Disturbances: Disrupted sleep patterns, insomnia, and sleep apnea can disrupt the body’s regulatory mechanisms, potentially leading to SVT episodes. Prioritizing healthy sleep habits promotes overall cardiovascular wellness.
Medication Interactions: Interactions between medications, both prescription and over-the-counter, can affect heart rhythm and increase susceptibility to SVT. Consulting healthcare providers about medication management is vital for SVT patients.
Preventive Measures And Management Strategies
Lifestyle Modifications: Adopting a heart-healthy lifestyle comprising balanced nutrition, regular exercise, stress management techniques, and adequate sleep can significantly reduce SVT triggers.
Medication Management: For individuals requiring medication for SVT control, adherence to prescribed regimens and awareness of potential interactions with other medications are paramount.
Electrophysiology Studies (EPS) and Ablation: In cases where SVT episodes are frequent or resistant to conservative measures, electrophysiology studies and catheter ablation may be recommended to identify and correct abnormal electrical pathways in the heart.
Regular Monitoring and Follow-Up: Maintaining regular follow-ups with cardiologists or electrophysiologists for ongoing monitoring, evaluation of triggers, and adjustment of management plans is essential for long-term SVT management.
By comprehensively exploring the diverse triggers of SVT episodes and emphasizing proactive management strategies, individuals can empower themselves to navigate SVT challenges effectively and enhance their cardiovascular well-being.
Identifying Personal Triggers
While the above triggers are common, it’s essential for individuals with SVT to identify their specific triggers. Keeping a detailed diary of activities, emotions, diet, and environmental factors can help pinpoint what sets off episodes. This information is valuable for healthcare providers in tailoring management strategies.
Management And Prevention Strategies
Once triggers are identified, the focus shifts to management and prevention strategies. These may include:
Lifestyle Modifications: Avoiding or moderating caffeine and alcohol consumption, quitting smoking, managing stress through techniques like mindfulness and relaxation exercises.
Medication Adjustment: Working with healthcare providers to adjust medications that may be triggering SVT episodes or switching to alternative medications.
Hydration and Electrolyte Balance: Ensuring adequate hydration and maintaining proper electrolyte balance through a balanced diet or supplements as recommended by healthcare providers.
Exercise Management: Engaging in regular exercise but avoiding intense or strenuous activities that may trigger SVT. Gradual warm-ups and cool-downs can be beneficial.
Avoiding Triggers: Once identified, actively avoiding known triggers can significantly reduce the frequency of SVT episodes.
Conclusion
Understanding what triggers an SVT episode is crucial for individuals living with this condition. By identifying and managing triggers, individuals can better control their symptoms and improve their quality of life. Working closely with healthcare providers to develop personalized management plans is key to effectively managing SVT and reducing its impact on daily activities.
FAQs
Is SVT dangerous?
SVT (Supraventricular Tachycardia) can be concerning but is not inherently life-threatening in most cases. However, its impact varies depending on several factors:
Frequency and Duration of Episodes: Frequent and prolonged SVT episodes can lead to symptoms like palpitations, dizziness, chest discomfort, and fatigue, affecting quality of life.
Underlying Health Conditions: Individuals with underlying heart conditions may experience more severe symptoms or complications from SVT.
Complications: While rare, complications like fainting (syncope) due to reduced blood flow during rapid heart rates can occur. In extreme cases, prolonged SVT can contribute to heart failure or increase the risk of stroke.
Treatment and Management: Proper diagnosis, understanding triggers, and implementing appropriate treatment strategies significantly reduce the risks associated with SVT. With timely intervention and lifestyle modifications, most individuals with SVT lead normal, healthy lives.
Will a fast heartbeat cause sudden death?
A fast heartbeat, especially during an SVT episode, can be unsettling. However, the likelihood of sudden death solely due to a fast heartbeat (tachycardia) is rare, particularly in isolated SVT cases without underlying cardiac issues. Factors that contribute to sudden cardiac death often involve more complex conditions such as severe coronary artery disease, structural heart abnormalities, or inherited arrhythmias like Long QT Syndrome or Brugada Syndrome.
These conditions may predispose individuals to dangerous arrhythmias that can lead to sudden cardiac arrest.Risk Factors for Sudden Cardiac Death: It’s crucial to recognize and address risk factors such as family history of sudden cardiac death, prior heart attacks, heart failure, and significant heart rhythm disorders. Managing these risk factors through medical supervision, lifestyle adjustments, and appropriate interventions reduces the likelihood of sudden cardiac death.
How is SVT treated?
Treatment for SVT focuses on controlling heart rate during episodes, preventing future episodes, and managing associated symptoms. Common approaches include:
Vagal Maneuvers: Techniques like the Valsalva maneuver (bearing down as if having a bowel movement), coughing forcefully, or plunging the face into ice water can help stimulate the vagus nerve and slow down the heart rate during an SVT episode.
Medications: Antiarrhythmic medications such as beta-blockers, calcium channel blockers, or adenosine may be prescribed to manage and prevent SVT episodes.
Catheter Ablation: In cases where medications are ineffective or poorly tolerated, catheter ablation may be recommended. This minimally invasive procedure involves mapping and ablating abnormal electrical pathways in the heart, effectively curing SVT in many cases.
Lifestyle Modifications: Adopting a heart-healthy lifestyle, avoiding known triggers, managing stress, maintaining a healthy weight, and quitting smoking contribute to SVT management and overall cardiovascular wellness.
Individualized Approach: Treatment plans for SVT are tailored to each patient’s unique circumstances, considering factors like frequency of episodes, symptom severity, underlying health conditions, and response to initial interventions.