Arrhythmia, characterized by irregular heartbeats, is a complex cardiovascular condition that raises concerns about its potential impact on health and well-being. Understanding the severity of arrhythmia and its potential to be life-threatening is crucial for individuals diagnosed with this condition and those seeking information about heart health. This article delves into the question of whether arrhythmia is life-threatening, exploring different types of arrhythmias, associated risks, and management strategies.
Understanding Arrhythmia
Arrhythmia refers to abnormal heart rhythms that can manifest as irregular heartbeats, skipped beats, or excessively rapid or slow beats. These irregularities can occur due to various factors, including issues with the heart’s electrical system, structural abnormalities, underlying health conditions, medication side effects, or lifestyle factors. Arrhythmias are classified based on where they originate in the heart (atria or ventricles) and their rhythm patterns.
Common Types of arrhythmias include:
Atrial Fibrillation (AFib): AFib is the most prevalent type of arrhythmia, characterized by irregular and rapid heartbeats originating in the heart’s upper chambers (atria). AFib can increase the risk of stroke, heart failure, and other cardiovascular complications.
Supraventricular Tachycardia (SVT): SVT involves rapid heartbeats originating above the ventricles, leading to episodes of sudden palpitations, chest discomfort, dizziness, and in some cases, fainting.
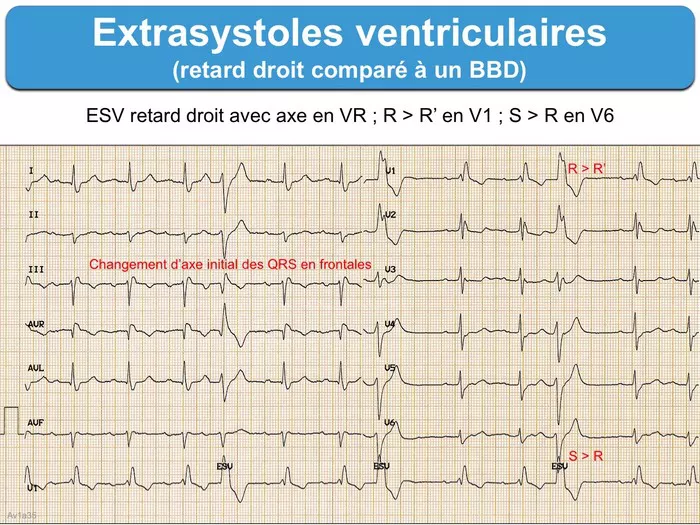
Ventricular Arrhythmias: This category includes conditions like ventricular tachycardia (VT) and ventricular fibrillation (VF), which involve rapid or chaotic heartbeats originating in the heart’s lower chambers (ventricles). Ventricular arrhythmias can be life-threatening and require immediate medical attention.
Bradycardia: In contrast to tachycardia, bradycardia is characterized by an abnormally slow heart rate, which can cause symptoms like fatigue, dizziness, fainting, and shortness of breath.
Assessing The Risk of Arrhythmia
The risk associated with arrhythmia varies depending on several factors, including the type of arrhythmia, the underlying cause, individual health status, presence of other cardiovascular conditions, and overall management strategies. Here’s a closer look at the potential risks associated with different types of arrhythmias:
Atrial Fibrillation (AFib): While AFib itself may not be immediately life-threatening, it can lead to serious complications that increase the risk of mortality. These complications include stroke (due to blood clots forming in the atria), heart failure (due to ineffective pumping of blood), and an increased risk of developing other heart rhythm disorders.
Supraventricular Tachycardia (SVT): SVT episodes can be distressing and may lead to complications such as fainting, chest pain, or reduced blood flow to vital organs. While SVT is generally not considered life-threatening in most cases, it can significantly impact quality of life and may require medical intervention to manage symptoms and prevent recurrence.
Ventricular Arrhythmias: Ventricular arrhythmias, particularly ventricular tachycardia (VT) and ventricular fibrillation (VF), are considered life-threatening emergencies. These arrhythmias can lead to sudden cardiac arrest, where the heart stops beating effectively, depriving the body of oxygen and leading to loss of consciousness or death if not treated promptly with CPR and defibrillation.
Bradycardia: In cases of severe bradycardia (very slow heart rate), there may be a risk of reduced blood flow to vital organs, leading to symptoms such as dizziness, fainting, or chest pain. While not all instances of bradycardia are life-threatening, individuals with significant bradycardia may require medical evaluation and intervention to address underlying causes and prevent complications.
Factors Influencing The Severity of Arrhythmia
Several factors can influence the severity and potential life-threatening nature of arrhythmia:
Underlying Heart Conditions: Individuals with pre-existing heart conditions, such as coronary artery disease, heart failure, cardiomyopathy, or structural heart defects, may be at higher risk for arrhythmia-related complications, including sudden cardiac arrest.
Electrolyte Imbalances: Abnormal levels of electrolytes (such as potassium, magnesium, or calcium) can disrupt the heart’s electrical activity and increase the risk of arrhythmias. Managing electrolyte imbalances is crucial for maintaining heart health.
Medications: Certain medications, including antiarrhythmic drugs, beta-blockers, calcium channel blockers, and diuretics, can affect heart rhythm and may increase or decrease the risk of arrhythmia-related complications. It’s essential for individuals to take medications as prescribed and report any adverse effects to their healthcare providers.
Lifestyle Factors: Factors such as smoking, excessive alcohol consumption, drug use, stress, poor diet, and lack of physical activity can contribute to the development or exacerbation of arrhythmias. Adopting heart-healthy lifestyle habits can help reduce the risk of arrhythmia and associated complications.
Managing Arrhythmia and Reducing Risks
Effective management of arrhythmia involves a comprehensive approach that addresses underlying causes, risk factors, and individual health needs. Key strategies for managing arrhythmia and reducing associated risks include:
Medical Evaluation: Individuals experiencing symptoms of arrhythmia, such as palpitations, chest pain, dizziness, fainting, or shortness of breath, should seek prompt medical evaluation. Diagnostic tests, including electrocardiograms (ECG or EKG), Holter monitoring, stress tests, echocardiograms, and electrophysiology studies, may be performed to assess heart rhythm and identify underlying issues.
Medication Management: Healthcare providers may prescribe medications to manage arrhythmia, control heart rate or rhythm, prevent blood clots (in cases of AFib), and reduce the risk of complications. It’s important to take medications as prescribed and attend regular follow-up appointments to monitor treatment effectiveness and adjust medications as needed.
Monitoring and Follow-Up: Regular monitoring of heart rhythm, blood pressure, and overall cardiovascular health is essential for individuals with arrhythmia. This may involve home monitoring with devices such as blood pressure monitors, heart rate monitors, or mobile health apps, as well as periodic check-ups and follow-up appointments with healthcare providers.
Emergency Preparedness: Individuals with a history of life-threatening arrhythmias or those at increased risk of sudden cardiac arrest should be educated about emergency response procedures, including CPR (cardiopulmonary resuscitation) and the use of automated external defibrillators (AEDs). Family members, caregivers, and close contacts should also be trained in these lifesaving techniques.
Conclusion
In conclusion, while arrhythmia can vary in severity and risk, certain types of arrhythmias, particularly ventricular arrhythmias like ventricular tachycardia (VT) and ventricular fibrillation (VF), can be life-threatening and require immediate medical attention. Other types of arrhythmias, such as atrial fibrillation (AFib) or supraventricular tachycardia (SVT), may not be immediately life-threatening but can lead to serious complications and impact quality of life if left untreated.
FAQs
Can I die from arrhythmia?
Arrhythmia can indeed be life-threatening, but it depends on various factors including the type and severity of the arrhythmia, overall health, and promptness of medical intervention. Some arrhythmias are benign and may not significantly impact health, while others can lead to serious complications such as cardiac arrest, which can be fatal if not treated promptly with CPR and defibrillation. It’s crucial for individuals with arrhythmias to work closely with healthcare professionals to manage their condition and reduce the risk of adverse outcomes.
What happens if the heart rate drops below 50?
If the heart rate drops below 50 beats per minute (BPM), it is considered bradycardia. While bradycardia can be normal for some individuals, especially athletes or those with good cardiovascular fitness, it can also indicate an underlying medical issue. Symptoms associated with bradycardia may include dizziness, fainting, fatigue, confusion, or shortness of breath.
Severe bradycardia can lead to reduced blood flow to vital organs and, in extreme cases, cardiac arrest.
If you experience symptoms or concerns related to a low heart rate, seek medical evaluation for proper diagnosis and management.
Will you definitely die if you have a heart attack?
Regarding heart attacks, not everyone who experiences a heart attack will die from it. Survival rates depend on various factors including the promptness of medical care, the severity of the heart attack, the individual’s overall health, and how quickly they receive treatments such as clot-dissolving medications or procedures like angioplasty and stenting.
Quick recognition of heart attack symptoms and immediate medical intervention significantly improve the chances of survival and reduce the risk of long-term complications. It’s essential to seek emergency medical help if you suspect a heart attack to receive timely treatment and improve outcomes.