Atrial fibrillation (AFib) is a common cardiac arrhythmia characterized by irregular and often rapid heartbeats. While AFib primarily affects the heart’s rhythm, its impact can extend beyond the cardiovascular system, leading to symptoms such as dizziness. Understanding why atrial fibrillation causes dizziness involves delving into the complex interplay between the heart’s electrical activity, blood flow, and neurological responses. This article explores the mechanisms behind dizziness in atrial fibrillation, its clinical significance, and management strategies for individuals living with this condition.
The Heart’s Electrical Chaos
Atrial fibrillation disrupts the heart’s normal electrical signals, causing the atria (upper chambers) to quiver irregularly instead of contracting effectively. This chaotic electrical activity can result in rapid and erratic heartbeats, leading to hemodynamic instability. The irregular heartbeat pattern in AFib reduces the heart’s efficiency in pumping blood, affecting circulation throughout the body.
Impaired Blood Flow And Oxygen Delivery
One of the critical consequences of atrial fibrillation is the compromised blood flow. The irregular contractions of the atria can lead to blood pooling in the chambers, especially the left atrial appendage. This stagnant blood increases the risk of clot formation, which can subsequently lead to embolic events like strokes.
Moreover, the irregular heart rhythm in AFib impairs the heart’s ability to adequately perfuse organs and tissues with oxygenated blood. This reduced oxygen delivery can affect various systems, including the brain, contributing to symptoms like dizziness and lightheadedness.
Neurological Responses to Altered Circulation
The brain plays a central role in regulating blood pressure and maintaining equilibrium. In atrial fibrillation, the irregular heartbeat and impaired circulation can trigger abnormal neurological responses, leading to dizziness. These responses include:
Orthostatic Hypotension: Changes in posture, such as standing up quickly, can exacerbate dizziness in individuals with AFib. Orthostatic hypotension refers to a sudden drop in blood pressure upon standing, leading to lightheadedness or fainting.
Baroreceptor Dysfunction: Baroreceptors are specialized sensors that detect changes in blood pressure. In AFib, the rapid and irregular heartbeats can disrupt the baroreceptor reflex, causing fluctuations in blood pressure and contributing to dizziness.
Cerebral Perfusion Changes: The irregular blood flow associated with atrial fibrillation can affect cerebral perfusion, impacting oxygen and nutrient delivery to the brain. This altered perfusion can manifest as dizziness and cognitive symptoms.
Impact of Underlying Conditions
Atrial fibrillation often coexists with other cardiovascular and systemic conditions, amplifying the risk of dizziness. Common comorbidities include:
Hypertension: High blood pressure can exacerbate cardiovascular strain and contribute to dizziness episodes.
Coronary Artery Disease: Reduced blood flow to the heart muscle can worsen symptoms during AFib episodes.
Valvular Heart Disease: Structural abnormalities in heart valves can further impair cardiac function and circulation.
Diabetes: Uncontrolled diabetes can affect neurological function and exacerbate dizziness symptoms.
Diagnostic Evaluation And Management
Diagnosing the underlying cause of dizziness in individuals with atrial fibrillation requires a comprehensive assessment, including:
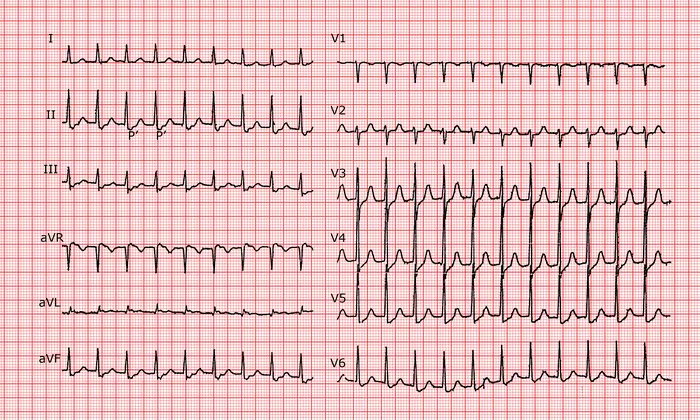
Electrocardiogram (ECG) to confirm AFib and assess heart rate and rhythm.
Holter monitoring or event recording to capture intermittent arrhythmias and correlate with symptoms.
Echocardiography to evaluate cardiac structure and function, assessing for structural abnormalities or valvular disease.
Management strategies for dizziness in atrial fibrillation encompass:
Rate and Rhythm Control: Controlling heart rate and restoring normal sinus rhythm can improve cardiac output and reduce dizziness episodes.
Anticoagulation Therapy: Managing clot formation with anticoagulants is crucial to prevent embolic complications like strokes.
Blood Pressure Management: Optimizing blood pressure control can minimize orthostatic hypotension and associated dizziness.
Lifestyle Modifications: Encouraging a healthy lifestyle with regular exercise, balanced nutrition, and stress management can support overall cardiovascular health.
Symptom Monitoring: Regular follow-up visits with healthcare providers to monitor symptoms, adjust medications, and assess treatment efficacy.
Conclusion
Atrial fibrillation can lead to dizziness through a combination of impaired cardiac function, altered circulation, and neurological responses. Understanding the mechanisms underlying dizziness in AFib is essential for accurate diagnosis, effective management, and improving the quality of life for individuals living with this arrhythmia. Collaborative efforts between patients, healthcare providers, and specialists are crucial in addressing the multifaceted aspects of atrial fibrillation and its associated symptoms.
FAQs
Is atrial fibrillation life-threatening?
Atrial fibrillation (AFib) can be life-threatening, especially if left untreated or if it leads to complications like stroke or heart failure. It’s important to manage AFib properly with medication, lifestyle changes, and sometimes medical procedures to reduce the risk of serious complications.
What does atrial fibrillation feel like?
The experience of atrial fibrillation can vary from person to person. Some common sensations include palpitations (rapid, irregular heartbeat), shortness of breath, fatigue, chest discomfort, and dizziness. However, not everyone with AFib experiences symptoms, which is why regular check-ups are crucial for early detection and management.
Does atrial fibrillation require surgery?
In terms of treatment, not everyone with AFib requires surgery. The approach to managing AFib depends on factors like the severity of symptoms, underlying health conditions, and the risk of complications. Treatment options can include medication to control heart rate or rhythm, procedures like cardioversion to restore normal heart rhythm, catheter ablation to treat underlying heart issues, or in some cases, surgery may be considered if other treatments are not effective. It’s important for individuals with AFib to work closely with their healthcare providers to determine the best treatment plan for their specific situation.