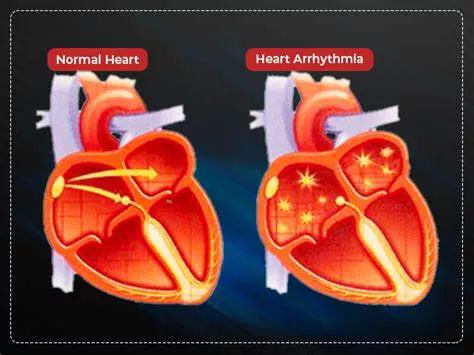
Cardiac arrhythmias, also known simply as heart arrhythmias, encompass a range of conditions characterized by an irregular heartbeat, which can be either too fast, too slow, or erratic. While many arrhythmias are benign, some are lethal and require immediate medical attention. Understanding these lethal arrhythmias is crucial for both medical professionals and the public to ensure timely intervention and management. This article will delve into the five lethal arrhythmias, discussing their mechanisms, clinical presentations, management strategies, and the importance of early detection and treatment.
The Five Lethal Arrhythmias
1. Ventricular Fibrillation (VF)
Ventricular fibrillation is arguably the most critical and immediately life-threatening arrhythmia. It occurs when the electrical activity within the ventricles becomes so chaotic that the heart ceases to pump blood effectively, leading to sudden cardiac arrest. The ventricular muscle fibers contract independently and rapidly, resulting in quivering rather than effective pumping.
Mechanism: VF typically arises due to ischemic heart disease, myocardial infarction (heart attack), or cardiomyopathies, although it can also occur due to electrolyte imbalances, drug toxicity, or severe hypothermia.
Clinical Presentation: Patients with VF will suddenly lose consciousness due to the lack of effective blood flow. This condition manifests without a pulse or blood pressure and requires immediate cardiopulmonary resuscitation (CPR) and defibrillation.
Management: The management of VF involves immediate resuscitation, including the use of automated external defibrillators (AEDs) to deliver shocks and restore normal heart rhythm. Early defibrillation, within the first few minutes following the onset of VF, significantly increases the chances of survival and recovery.
2. Ventricular Tachycardia (VT)
Ventricular tachycardia is characterized by a fast heart rate that originates from the ventricles and can be potentially life-threatening, especially if sustained or associated with underlying cardiac conditions.
Mechanism: VT often develops in the setting of structural heart disease, such as previous myocardial infarction, where scar tissue in the ventricles facilitates abnormal electrical pathways. Other causes include drug toxicity, electrolyte disturbances, and genetic disorders affecting cardiac ion channels.
Clinical Presentation: VT may be asymptomatic in some cases but often presents with palpitations, dizziness, syncope, or cardiac arrest, depending on the rate and duration of the tachycardia and the patient’s underlying cardiac health.
Management: Treatment of VT involves both acute and long-term strategies, including antiarrhythmic drugs, electrical cardioversion if the patient is unstable, and potentially catheter ablation to remove the abnormal electrical pathway.
Implantable cardioverter-defibrillators (ICDs) are often recommended for patients at high risk of recurrent VT.
3. Torsade De Pointes (TdP)
Torsade de Pointes is a unique form of polymorphic ventricular tachycardia that typically occurs in the context of a prolonged QT interval on the electrocardiogram (ECG). It can degenerate into VF and lead to sudden cardiac death.
Mechanism: TdP is frequently triggered by medications that prolong the QT interval, electrolyte imbalances (particularly low levels of potassium and magnesium), and genetic disorders such as congenital long QT syndrome.
Clinical Presentation: Patients may experience sudden, brief episodes of dizziness, palpitations, or syncope. TdP can swiftly progress to VF if not treated promptly.
Management: The management of TdP includes immediate magnesium sulfate administration, correction of electrolyte imbalances, and avoidance of QT-prolonging drugs. In cases of recurrent TdP, temporary pacing or isoproterenol infusion may be necessary to increase the heart rate and prevent recurrences.
4. Atrial Fibrillation (AF) with Rapid Ventricular Response
Atrial fibrillation itself is not typically life-threatening, but it can become dangerous when associated with a rapid ventricular response (RVR), leading to hemodynamic instability.
Mechanism: AF with RVR occurs when the atria beat chaotically, leading to irregular conduction to the ventricles which then respond by increasing the heart rate. This can severely impair cardiac output, especially in patients with pre-existing heart disease.
Clinical Presentation: Symptoms include palpitations, fatigue, shortness of breath, chest pain, and in severe cases, hypotension and heart failure.
Management: Management strategies focus on rate control using medications such as beta-blockers or calcium channel blockers. In cases where rate control is inadequate, rhythm control through electrical cardioversion may be necessary.
Anticoagulation is also crucial to prevent stroke due to the increased risk of thromboembolism in AF.
5. Complete Heart Block (Third-Degree AV Block)
Complete heart block is a severe type of conduction block where no atrial impulses pass through to the ventricles. This can lead to a dangerously slow heart rate and inadequate cardiac output.
Mechanism: Third-degree AV block may result from degenerative changes in the conduction system, myocardial infarction, congenital defects, or as a side effect of medications such as beta-blockers or digoxin.
Clinical Presentation: Patients may present with fatigue, dizziness, episodes of syncope, or in extreme cases, sudden cardiac arrest.
Management: The definitive treatment for complete heart block is the implantation of a pacemaker, which provides reliable pacing to maintain adequate heart rates and cardiac output. In acute settings, temporary pacing may be needed until permanent pacemaker placement can be arranged.
Conclusion
The five lethal arrhythmias outlined above underscore the importance of early recognition, prompt intervention, and specialized management to reduce morbidity and mortality associated with these conditions. Public awareness campaigns and education for healthcare providers on the swift recognition and management of arrhythmias can significantly improve patient outcomes. As medical technology and research advance, further improvements in the diagnosis, treatment, and prevention of lethal arrhythmias continue to evolve, offering hope for better management and survival rates for patients affected by these serious conditions.