Atrial fibrillation (AFib) is a common heart condition that affects millions of people worldwide. It is characterized by an irregular and often rapid heart rate, which can lead to various symptoms and complications. One of the most concerning and uncomfortable symptoms associated with AFib is chest pain. Understanding why AFib causes chest pain is crucial for managing the condition effectively and reducing the risk of serious complications.
Understanding Atrial Fibrillation
Atrial fibrillation occurs when the electrical signals in the atria (the upper chambers of the heart) become chaotic, leading to an irregular and often fast heartbeat. This irregularity disrupts the normal rhythm and coordination of the heart, affecting its ability to pump blood efficiently. There are several types of AFib, including paroxysmal (intermittent), persistent (lasting longer than a week), and permanent (continuous). Regardless of the type, AFib can have significant implications for cardiovascular health.
The Connection Between AFib and Chest Pain
1. Reduced Blood Flow to the Heart
One of the primary reasons AFib causes chest pain is due to reduced blood flow to the heart muscle. During AFib, the heart’s upper chambers quiver instead of contracting effectively. This quivering results in an incomplete emptying of the atria, leading to decreased cardiac output. When the heart cannot pump blood efficiently, less oxygen-rich blood reaches the coronary arteries that supply the heart muscle. This condition, known as myocardial ischemia, can cause chest pain or angina.
2. Increased Heart Rate and Workload
AFib often leads to a rapid and irregular heart rate. This increased heart rate means the heart is working harder than usual, leading to increased oxygen demand by the heart muscle. When the heart’s workload exceeds its oxygen supply, it can cause ischemia and chest pain. The sensation of chest pain in this context is similar to what occurs during a heart attack, although the underlying mechanisms differ.
3. Formation of Blood Clots
AFib can increase the risk of blood clot formation within the atria. When the atria do not contract effectively, blood can pool and stagnate, leading to the formation of clots. If a clot breaks loose and travels to the coronary arteries, it can obstruct blood flow, resulting in a condition known as coronary artery embolism. This blockage can cause chest pain and, if not promptly treated, may lead to a heart attack.
4. Structural Changes in the Heart
Chronic AFib can lead to structural changes in the heart, such as atrial enlargement and fibrosis (scarring). These changes can further impair the heart’s function and contribute to symptoms like chest pain. The enlargement of the atria can put additional strain on the heart muscle and the surrounding structures, leading to discomfort and pain.
5. Increased Anxiety and Stress
Living with AFib can be stressful and anxiety-inducing. Anxiety and stress are known to exacerbate cardiovascular symptoms, including chest pain. The fear of experiencing an AFib episode or the uncertainty of its onset can lead to heightened anxiety, which in turn can trigger or worsen chest pain. This psychosomatic response can create a vicious cycle where anxiety leads to chest pain, and chest pain increases anxiety.
Recognizing and Managing AFib-Related Chest Pain
1. Symptom Awareness
Being aware of the symptoms associated with AFib, including chest pain, is crucial for timely intervention. Chest pain in AFib may vary in intensity and duration. It can be sharp, dull, or aching and may be accompanied by other symptoms such as shortness of breath, palpitations, dizziness, or fatigue. Recognizing these symptoms and seeking medical attention promptly can prevent complications.
2. Medical Evaluation and Diagnosis
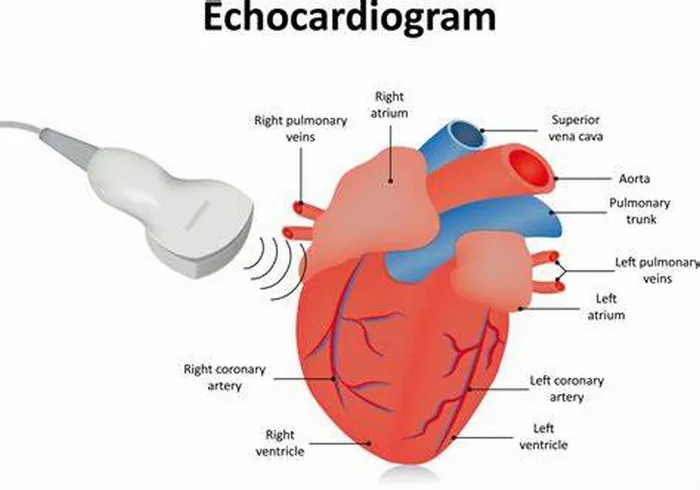
A thorough medical evaluation is essential to determine the cause of chest pain in individuals with AFib. Healthcare providers may use various diagnostic tools, including electrocardiograms (ECGs), echocardiograms, stress tests, and blood tests, to assess the heart’s function and identify any underlying issues. Diagnosing the exact cause of chest pain helps in tailoring an appropriate treatment plan.
3. Medications and Treatment Options
Managing AFib and its associated chest pain often involves a combination of medications and lifestyle changes. Common medications used to treat AFib include:
Antiarrhythmic drugs: These medications help regulate the heart’s rhythm and prevent episodes of AFib.
Rate control drugs: Beta-blockers and calcium channel blockers are used to control the heart rate, reducing the workload on the heart.
Anticoagulants: These drugs prevent blood clots from forming and reduce the risk of stroke and other complications.
Nitrates: Used to relieve chest pain by dilating the coronary arteries and improving blood flow to the heart muscle.
In some cases, more invasive procedures may be necessary, such as cardioversion (electric shock to restore normal rhythm), catheter ablation (destroying abnormal heart tissue causing AFib), or surgical interventions like the Maze procedure.
4. Lifestyle Modifications
Making lifestyle changes can significantly impact the management of AFib and reduce the occurrence of chest pain. Some recommended lifestyle modifications include:
Diet: Eating a heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can improve cardiovascular health. Reducing salt intake and avoiding caffeine and alcohol can also help manage AFib.
Exercise: Regular physical activity, tailored to an individual’s fitness level, can improve heart health and reduce symptoms of AFib.
However, it is essential to consult with a healthcare provider before starting any exercise regimen.
Stress management: Techniques such as yoga, meditation, deep breathing exercises, and mindfulness can help reduce stress and anxiety, potentially decreasing the frequency and severity of chest pain.
Smoking cessation: Quitting smoking is crucial for overall heart health and can reduce the risk of AFib-related complications.
5. Regular Monitoring and Follow-Up
Regular monitoring and follow-up with a healthcare provider are essential for managing AFib and preventing complications. Continuous assessment of heart rhythm, medication effectiveness, and overall health can help detect any changes early and adjust treatment plans accordingly. Utilizing wearable devices that monitor heart rate and rhythm can provide valuable data for both patients and healthcare providers.
Conclusion
Atrial fibrillation is a complex condition that can significantly impact an individual’s quality of life. Understanding why AFib causes chest pain involves recognizing the interplay between irregular heart rhythms, reduced blood flow, increased heart workload, and psychological factors. Proper management of AFib, through medications, lifestyle changes, and regular medical evaluation, can help alleviate chest pain and reduce the risk of serious complications. Individuals with AFib should work closely with their healthcare providers to develop a personalized treatment plan that addresses their specific needs and symptoms. By taking proactive steps and seeking appropriate care, those living with AFib can lead healthier and more comfortable lives.