Cardiomyopathy is a disease of the heart muscle that affects its ability to pump blood effectively. It can lead to heart failure, irregular heartbeats (arrhythmias), and other complications. There are several types of cardiomyopathy, each with distinct characteristics and causes. Understanding these types is crucial for diagnosis and treatment. The most common type of cardiomyopathy is dilated cardiomyopathy (DCM). This article explores the characteristics, causes, symptoms, diagnosis, treatment, and management of dilated cardiomyopathy, along with its impact on patients’ lives.
What Is Cardiomyopathy?
Cardiomyopathy encompasses a group of diseases that affect the heart muscle, often leading to a weakened heart that struggles to pump blood effectively. The main types of cardiomyopathy include:
- Dilated Cardiomyopathy (DCM)
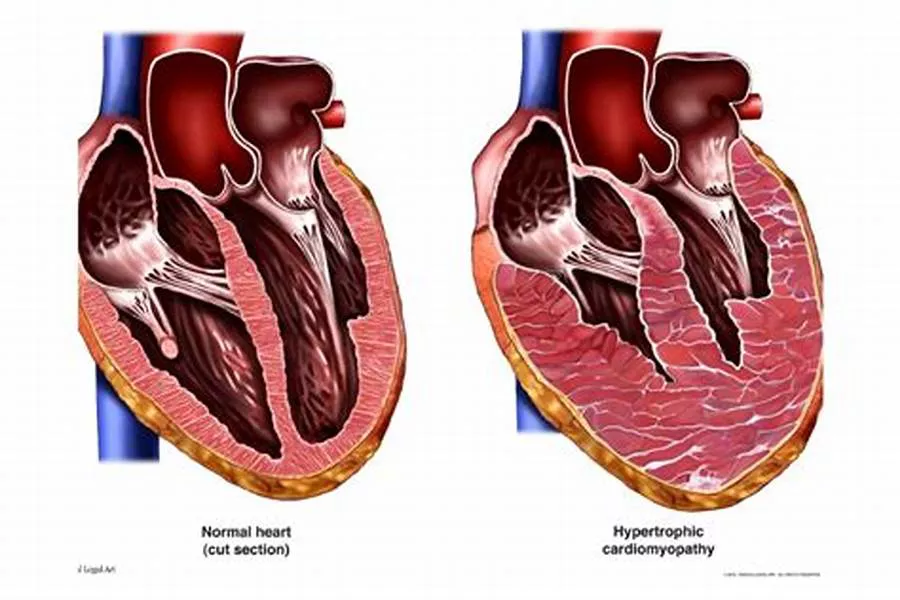
- Hypertrophic Cardiomyopathy (HCM)
- Restrictive Cardiomyopathy (RCM)
- Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC)
- Takotsubo Cardiomyopathy
Each type has unique features, but dilated cardiomyopathy stands out as the most prevalent.
What Is Dilated Cardiomyopathy?
Dilated cardiomyopathy (DCM) is characterized by the enlargement and weakening of the left ventricle, the heart’s main pumping chamber. This enlargement leads to a reduced ability to pump blood, which can cause heart failure and other complications.
Causes of Dilated Cardiomyopathy
The exact cause of DCM often remains unknown (idiopathic), but several factors can contribute to its development:
Genetic Predisposition: Genetic mutations are found in approximately 30-40% of DCM cases, making family history a significant risk factor.
Infections: Viral infections, such as myocarditis, can damage the heart muscle.
Alcohol Abuse: Chronic excessive alcohol consumption can lead to alcohol-induced cardiomyopathy, a subset of DCM.
Drug Toxicity: Certain chemotherapy drugs and other medications can be toxic to the heart muscle.
Nutritional Deficiencies: Deficiencies in nutrients like thiamine can cause beriberi heart disease, a form of DCM.
Autoimmune Diseases: Conditions like lupus can cause inflammation and damage to the heart muscle.
Endocrine Disorders: Diabetes, thyroid disease, and other endocrine disorders can contribute to DCM.
Symptoms of Dilated Cardiomyopathy
DCM can present with a variety of symptoms, which often develop gradually:
Shortness of Breath:This is particularly noticeable during physical activity or when lying down.
Fatigue: Reduced blood flow can lead to persistent tiredness.
Swelling: Edema in the legs, ankles, and feet is common due to fluid retention.
Chest Pain: Some patients may experience chest discomfort.
Arrhythmias: Irregular heartbeats, including atrial fibrillation and ventricular tachycardia, can occur.
Syncope: Fainting or lightheadedness can result from poor blood flow to the brain.
Diagnosing Dilated Cardiomyopathy
Diagnosing DCM involves a combination of medical history, physical examination, and various diagnostic tests:
Echocardiogram: This ultrasound test provides detailed images of the heart’s structure and function, revealing dilation and weakened contractions.
Electrocardiogram (ECG): An ECG records the electrical activity of the heart and can detect arrhythmias or other abnormalities.
Chest X-ray: An X-ray can show the size and shape of the heart and detect fluid in the lungs.
Cardiac MRI: This imaging test provides detailed images of the heart muscle and can identify scarring or other structural changes.
Blood Tests: Tests can identify markers of heart failure, such as elevated B-type natriuretic peptide (BNP) levels, and other conditions like thyroid disease or infections.
Genetic Testing: In familial cases, genetic testing can identify mutations associated with DCM.
Treatment of Dilated Cardiomyopathy
Treatment for DCM aims to improve symptoms, prevent complications, and enhance quality of life. It often involves a combination of lifestyle changes, medications, and in some cases, surgical interventions:
Lifestyle Modifications:
Diet: A heart-healthy diet low in sodium and saturated fats can help manage symptoms.
Exercise:Regular, moderate exercise can improve cardiovascular health, but patients should avoid strenuous activities.
Alcohol and Tobacco: Avoiding alcohol and quitting smoking are crucial steps.
Medications:
ACE Inhibitors: These drugs relax blood vessels, reduce blood pressure, and decrease the heart’s workload.
Beta-Blockers: These medications slow the heart rate and reduce blood pressure.
Diuretics: Diuretics help eliminate excess fluid and reduce swelling.
Aldosterone Antagonists: These drugs help control fluid retention and improve heart function.
Anticoagulants: In patients with arrhythmias, anticoagulants prevent blood clots and reduce the risk of stroke.
Implantable Devices:
Implantable Cardioverter-Defibrillators (ICDs): These devices monitor heart rhythms and deliver shocks to correct life-threatening arrhythmias.
Cardiac Resynchronization Therapy (CRT): CRT devices coordinate the contractions of the heart’s ventricles, improving efficiency and function.
Surgical Options:
Heart Transplant: In severe cases, a heart transplant may be necessary.
Left Ventricular Assist Devices (LVADs): LVADs help the heart pump blood and are used as a bridge to transplant or as long-term therapy.
Managing Dilated Cardiomyopathy
Managing DCM requires ongoing medical care and monitoring:
Regular Follow-Up: Patients need regular check-ups with a cardiologist to monitor heart function and adjust treatments as needed.
Symptom Tracking: Keeping track of symptoms and reporting any changes promptly can help manage the condition effectively.
Support Systems: Emotional and psychological support is crucial for patients and their families, as living with DCM can be challenging.
Prognosis And Quality of Life
The prognosis for DCM varies depending on the severity of the disease and the effectiveness of treatment. With appropriate management, many patients can lead relatively normal lives. However, some may experience progressive heart failure, necessitating advanced treatments like heart transplants.
Survival Rates: Advances in medical treatments have improved survival rates for DCM patients.
Quality of Life: Managing symptoms and preventing complications are key to maintaining a good quality of life. Patients are encouraged to engage in cardiac rehabilitation programs, which provide education and support.
Research And Future Directions
Ongoing research aims to better understand the genetic and molecular mechanisms underlying DCM, leading to more targeted therapies. Areas of focus include:
Genetic Studies: Identifying specific genetic mutations and their impact on DCM development.
Stem Cell Therapy: Exploring the potential of stem cell therapy to regenerate damaged heart tissue.
New Medications: Developing drugs that target the underlying causes of DCM rather than just managing symptoms.
Improved Diagnostics: Enhancing imaging techniques and biomarkers for earlier and more accurate diagnosis.
Conclusion
Dilated cardiomyopathy is the most common type of cardiomyopathy, characterized by an enlarged and weakened left ventricle. While the exact cause often remains unknown, various factors such as genetics, infections, and lifestyle choices can contribute to its development. Understanding the symptoms, diagnostic methods, treatment options, and management strategies is crucial for improving patient outcomes and quality of life. Advances in research continue to offer hope for more effective treatments and better prognosis for those living with this challenging condition.
FAQs
What Fruits Can You Eat to Protect Your Heart?
Fruits are an essential part of a heart-healthy diet. Here are some fruits that are particularly beneficial for heart health:
Berries: Berries such as strawberries, blueberries, raspberries, and blackberries are rich in antioxidants like anthocyanins, which can reduce inflammation and oxidative stress in the body. These compounds help protect the heart and improve arterial health.
Apples: Apples contain soluble fiber and flavonoids, which can lower cholesterol levels and reduce the risk of heart disease. The soluble fiber in apples helps reduce the absorption of cholesterol in the intestines.
Citrus Fruits: Oranges, grapefruits, lemons, and limes are high in vitamin C, fiber, and flavonoids, all of which contribute to heart health. Vitamin C is an antioxidant that helps prevent damage to the blood vessels and reduces the risk of heart disease.
Bananas: Bananas are a good source of potassium, an essential mineral for heart health. Potassium helps regulate blood pressure by balancing the effects of sodium in the body.
Avocados: While technically a fruit, avocados are high in monounsaturated fats, which can help lower bad cholesterol (LDL) levels and increase good cholesterol (HDL) levels. They also provide potassium and fiber.
Pomegranates: Pomegranates contain powerful antioxidants, including punicalagins and anthocyanins, which have been shown to reduce oxidative stress, lower blood pressure, and reduce plaque buildup in the arteries.
Grapes: Grapes, especially dark-colored ones, are rich in antioxidants like resveratrol, which can protect the heart by reducing inflammation and preventing blood clots.
Tomatoes: Tomatoes are high in lycopene, an antioxidant linked to lower levels of bad cholesterol (LDL) and a reduced risk of heart disease.
Is Coronary Heart Disease the Same as Heart Disease?
Coronary heart disease (CHD) is a specific type of heart disease, but it is not the same as heart disease in general. Here is the distinction:
Heart Disease: This is a broad term that encompasses various conditions affecting the heart and blood vessels. Heart disease includes coronary heart disease, arrhythmias (irregular heartbeats), heart valve problems, heart failure, and congenital heart defects.
Coronary Heart Disease (CHD): Also known as coronary artery disease (CAD), CHD specifically refers to the condition where the coronary arteries, which supply blood to the heart muscle, become narrowed or blocked due to the buildup of plaque (atherosclerosis). This can lead to angina (chest pain), heart attacks, and other complications.
In summary, coronary heart disease is a subset of heart disease. All cases of CHD are considered heart disease, but not all heart disease cases are CHD.
What Causes Angina?
Angina is a symptom of coronary heart disease and occurs when the heart muscle doesn’t get enough oxygen-rich blood.
The main causes of angina include:
Atherosclerosis: The buildup of fatty deposits (plaque) in the coronary arteries narrows the arteries and reduces blood flow to the heart muscle. This reduced blood flow can cause chest pain, especially during physical exertion or stress when the heart requires more oxygen.
Coronary Artery Spasm: Sometimes, the coronary arteries can temporarily tighten or spasm, reducing blood flow to the heart muscle. This type of angina, known as variant or Prinzmetal’s angina, often occurs at rest and can be triggered by stress, cold weather, smoking, or certain medications.
Microvascular Angina: This type of angina is caused by problems in the tiny arteries of the heart. Even though the main coronary arteries may not be significantly blocked, the small blood vessels may not function properly, reducing blood flow to the heart muscle.
Other Causes: Conditions that increase the heart’s oxygen demand, such as high blood pressure, rapid heart rate (tachycardia), or severe anemia, can also cause angina by straining the heart’s ability to receive adequate blood supply.