Cardiomyopathy refers to diseases of the heart muscle that impair its ability to pump blood effectively. This condition can result from various factors, including genetic predispositions, long-term high blood pressure, heart valve problems, metabolic disorders, or exposure to toxins. The recovery time for cardiomyopathy varies greatly depending on the type and severity of the disease, the patient’s overall health, and the treatment strategies employed.
Types of Cardiomyopathy
Understanding the type of cardiomyopathy is crucial in estimating recovery time. There are four main types:
1. Dilated Cardiomyopathy (DCM)
Dilated cardiomyopathy is characterized by an enlarged and weakened heart. This type is often caused by coronary artery disease, alcohol abuse, or genetic factors. Recovery in DCM is often gradual and may require long-term treatment.
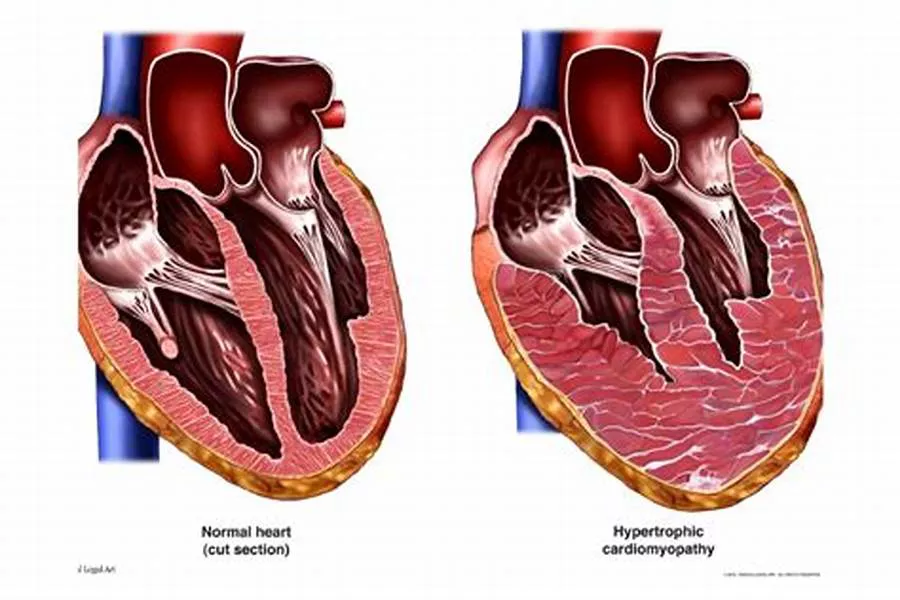
2. Hypertrophic Cardiomyopathy (HCM)
Hypertrophic cardiomyopathy involves abnormal thickening of the heart muscle, which can obstruct blood flow. This type is usually genetic. Recovery can be challenging, especially if symptoms are severe or if surgical intervention is needed.
3. Restrictive Cardiomyopathy (RCM)
Restrictive cardiomyopathy results from rigid heart walls that restrict the heart’s ability to fill with blood. This type can be caused by conditions like amyloidosis or sarcoidosis. Recovery can be slow and is often dependent on managing the underlying cause.
4. Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC)
Arrhythmogenic right ventricular cardiomyopathy involves the replacement of heart muscle with fatty or fibrous tissue, which can lead to arrhythmias. It is usually genetic. Recovery can vary, with some patients requiring devices like defibrillators.
Factors Influencing Recovery Time
Several factors influence the recovery time for cardiomyopathy:
Severity of the Condition
The severity of cardiomyopathy at diagnosis plays a significant role in recovery. Mild cases with few symptoms may see quicker improvement with treatment, while severe cases with extensive heart damage may require prolonged recovery periods.
Patient’s Overall Health
A patient’s general health, including the presence of other conditions such as diabetes, hypertension, or obesity, can affect recovery. Patients in good health aside from cardiomyopathy may recover faster than those with multiple health issues.
Typical Recovery Timeframes
Acute Phase (First Few Weeks to Months)
In the acute phase, the focus is on stabilizing the patient’s condition. This may involve hospitalization, intensive monitoring, and the initiation of treatments such as medications to improve heart function, reduce fluid buildup, and control blood pressure.
Subacute Phase (3 to 6 Months)
During the subacute phase, patients often continue with medical therapy and begin cardiac rehabilitation. Cardiac rehab involves supervised exercise, education on heart-healthy living, and counseling to reduce stress. Improvement in symptoms and heart function can typically be observed during this period.
Chronic Phase (6 Months and Beyond)
Recovery in the chronic phase is ongoing. Patients may see gradual improvements in heart function and symptoms over many months to years. Continuous monitoring and adjustments to treatment are essential. Some patients may achieve significant recovery, while others may need long-term management of their condition.
Lifestyle Modifications to Aid Recovery
Dietary Changes
Adopting a heart-healthy diet can help manage cardiomyopathy. This includes reducing salt intake to prevent fluid retention, eating plenty of fruits and vegetables, and avoiding foods high in saturated fat and cholesterol.
Regular Exercise
Engaging in regular, moderate exercise can improve cardiovascular health. Cardiac rehabilitation programs often include exercise plans tailored to individual needs and capabilities.
Avoiding Alcohol and Tobacco
Alcohol and tobacco can exacerbate heart conditions. Avoiding these substances is crucial for recovery.
Managing Stress
Chronic stress can negatively impact heart health. Techniques such as meditation, yoga, and deep-breathing exercises can help manage stress levels.
Medical Treatments And Interventions
Medications
Several medications can help manage cardiomyopathy symptoms and improve heart function:
Beta-Blockers: Reduce heart rate and blood pressure, easing the heart’s workload.
ACE Inhibitors: Help relax blood vessels and improve blood flow.
Diuretics: Help reduce fluid buildup in the body.
Anticoagulants: Prevent blood clots that could lead to stroke.
Surgical Interventions
In severe cases, surgical interventions may be necessary:
Implantable Devices: Pacemakers or defibrillators can help manage abnormal heart rhythms.
Septal Myectomy: Surgery to remove part of the thickened heart muscle in HCM.
Heart Transplant: In end-stage cardiomyopathy, a heart transplant may be the only option.
Monitoring and Follow-Up
Regular follow-up with a cardiologist is crucial to monitor the progress and adjust treatment as needed. This may involve periodic imaging tests like echocardiograms and stress tests to assess heart function.
Conclusion
Recovery from cardiomyopathy is a highly individualized process that depends on various factors, including the type and severity of the disease, the effectiveness of treatment, and the patient’s overall health and adherence to their treatment plan. While some patients may see significant improvement within a few months, others may require ongoing management and longer recovery periods.