Left ventricular failure, also known as left-sided heart failure, occurs when the left ventricle, the heart’s primary pumping chamber, is unable to effectively pump blood to the body. This condition leads to a cascade of symptoms and complications as the body struggles to maintain adequate circulation. Understanding the signs of left ventricular failure is crucial for timely diagnosis and treatment, potentially improving outcomes and quality of life for affected individuals.
What Are The Signs of Left Ventricular Failure?
Left ventricular failure manifests through a variety of symptoms that arise from the heart’s inability to effectively pump blood. These signs can be categorized into those resulting from congestion and those resulting from inadequate perfusion.
Congestion-Related Symptoms
When the left ventricle fails to pump blood efficiently, blood backs up into the lungs, leading to congestion-related symptoms:
Shortness of Breath (Dyspnea): One of the most common symptoms, shortness of breath occurs due to fluid accumulation in the lungs (pulmonary congestion). This can be particularly noticeable during physical activity (exertional dyspnea) or when lying flat (orthopnea). In severe cases, individuals may wake up suddenly during the night gasping for air, a condition known as paroxysmal nocturnal dyspnea.
Persistent Cough or Wheezing: A chronic cough, often producing white or pink frothy sputum, can be a sign of fluid in the lungs. Wheezing may also occur as the airways become narrowed due to congestion.
Pulmonary Edema: Acute episodes of fluid accumulation in the lungs can lead to severe shortness of breath, coughing up frothy sputum, and a feeling of drowning. Pulmonary edema is a medical emergency requiring immediate attention.
Nocturia: Increased urination at night is common in individuals with left ventricular failure. This occurs as the body attempts to eliminate excess fluid during periods of rest when cardiac output improves slightly.
Fatigue and Weakness: Due to reduced oxygen delivery to tissues, individuals often feel fatigued and weak, even with minimal exertion.
Weight Gain and Swelling (Edema): Fluid retention can lead to rapid weight gain and swelling in the legs, ankles, and feet. In some cases, abdominal swelling (ascites) may also occur.
Inadequate Perfusion Symptoms
Reduced cardiac output affects the delivery of oxygen and nutrients to tissues, leading to symptoms related to inadequate perfusion:
Exercise Intolerance: Individuals with left ventricular failure often experience a reduced ability to engage in physical activities. They may tire easily and find it difficult to perform routine tasks.
Cool Extremities: Poor blood flow can cause the skin, particularly on the hands and feet, to feel cool to the touch. This is due to the body prioritizing blood flow to vital organs.
Dizziness and Confusion: Insufficient blood flow to the brain can lead to dizziness, lightheadedness, and confusion. In severe cases, it may cause fainting (syncope).
Chest Pain (Angina): Some individuals may experience chest pain due to reduced blood flow to the heart itself. This symptom requires immediate medical evaluation to rule out other serious conditions like myocardial infarction.
Palpitations: Abnormal heart rhythms (arrhythmias) are common in heart failure and can cause a sensation of skipped beats or fluttering in the chest.
Underlying Causes And Risk Factors
Left ventricular failure can result from a variety of underlying conditions that damage or stress the heart. Common causes and risk factors include:
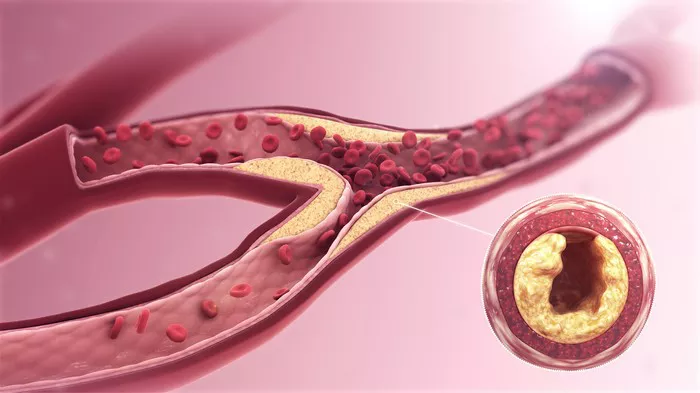
Coronary Artery Disease (CAD): Blockages in the coronary arteries reduce blood flow to the heart muscle, leading to ischemia and weakening of the left ventricle.
Hypertension (High Blood Pressure): Chronic high blood pressure forces the left ventricle to work harder, leading to hypertrophy (thickening of the heart muscle) and eventually to heart failure.
Myocardial Infarction (Heart Attack): Damage to the heart muscle from a heart attack can impair the left ventricle’s ability to pump blood.
Cardiomyopathy: Diseases of the heart muscle, such as dilated, hypertrophic, or restrictive cardiomyopathy, can weaken the left ventricle.
Valvular Heart Disease: Conditions affecting the heart valves, such as aortic stenosis or mitral regurgitation, can lead to increased workload and subsequent failure of the left ventricle.
Diabetes: Diabetes is a significant risk factor for heart failure due to its association with coronary artery disease and hypertension.
Lifestyle Factors: Smoking, obesity, sedentary lifestyle, and excessive alcohol consumption can all contribute to the development of left ventricular failure.
Diagnosis of Left Ventricular Failure
Diagnosing left ventricular failure involves a combination of medical history, physical examination, and diagnostic tests:
Medical History and Physical Examination: A detailed history of symptoms, risk factors, and family history of heart disease is taken. During the physical examination, signs such as crackles in the lungs, elevated jugular venous pressure, and peripheral edema may be noted.
Electrocardiogram (ECG): This test records the electrical activity of the heart and can help identify arrhythmias, ischemia, and other abnormalities.
Chest X-ray: A chest X-ray can reveal signs of pulmonary congestion, cardiomegaly (enlarged heart), and pleural effusion.
Echocardiogram: An echocardiogram uses ultrasound waves to create images of the heart, providing detailed information about the size, structure, and function of the left ventricle and other heart chambers.
Blood Tests: Blood tests, including B-type natriuretic peptide (BNP) or N-terminal pro-BNP (NT-proBNP) levels, can help diagnose and assess the severity of heart failure.
Cardiac MRI: Magnetic resonance imaging can provide detailed images of the heart’s structure and function, helping to identify underlying causes of left ventricular failure.
Stress Test: A stress test evaluates the heart’s response to physical exertion and can help diagnose ischemic heart disease.
Conclusion
Left ventricular failure is a serious condition that requires prompt diagnosis and comprehensive management. Recognizing the signs of left ventricular failure, such as shortness of breath, persistent cough, fatigue, and edema, is crucial for seeking timely medical attention. With appropriate treatment and lifestyle changes, individuals with left ventricular failure can manage their symptoms, improve their quality of life, and reduce the risk of complications. Understanding the underlying causes and risk factors, along with regular monitoring and adherence to treatment plans, plays a vital role in the effective management of this condition.
FAQs
what Treatment of Left Ventricular Failure
Treatment for left ventricular failure aims to alleviate symptoms, improve quality of life, and address the underlying cause.
The treatment plan may include:
Medications: Commonly prescribed medications include:
ACE Inhibitors or ARBs: These drugs help relax blood vessels and reduce the workload on the heart.
Beta-Blockers: Beta-blockers slow the heart rate and reduce blood pressure, decreasing the heart’s demand for oxygen.
Diuretics: Diuretics help remove excess fluid from the body, reducing congestion and edema.
Aldosterone Antagonists: These medications help prevent fluid retention and reduce the risk of hospitalization.
Digitalis: Digitalis can improve the heart’s pumping ability and control heart rate.
Lifestyle Modifications: Patients are encouraged to adopt a heart-healthy lifestyle, including:
Diet: A low-sodium diet helps prevent fluid retention. A balanced diet rich in fruits, vegetables, whole grains, and lean proteins supports overall heart health.
Exercise: Regular physical activity, tailored to the individual’s capacity, can improve cardiovascular fitness and reduce symptoms.
Weight Management: Maintaining a healthy weight reduces the strain on the heart.
Smoking Cessation: Quitting smoking improves cardiovascular health and reduces the risk of further heart damage.
Alcohol Limitation: Reducing alcohol intake can help prevent further weakening of the heart muscle.
Surgical and Interventional Procedures: In some cases, surgical or interventional procedures may be necessary:
Coronary Artery Bypass Grafting (CABG): This surgery improves blood flow to the heart by bypassing blocked coronary arteries.
Valve Repair or Replacement: Surgical intervention to repair or replace damaged heart valves can improve heart function.
Implantable Devices: Devices such as implantable cardioverter-defibrillators (ICDs) or cardiac resynchronization therapy (CRT) can help manage arrhythmias and improve heart function.
Advanced Therapies: For patients with severe heart failure, advanced therapies may be considered:
Left Ventricular Assist Device (LVAD): An LVAD is a mechanical pump that helps the left ventricle pump blood to the body.
Heart Transplant: In cases of end-stage heart failure, a heart transplant may be the best option for long-term survival and quality of life.
How long can you live with heart failure?
The prognosis for individuals with heart failure varies widely and depends on several factors, including the severity of the condition, the patient’s age, underlying health issues, and how well they adhere to their treatment plan.
Severity of Heart Failure: Heart failure is classified into stages (A to D) and functional classes (I to IV) by the American College of Cardiology/American Heart Association (ACC/AHA) and the New York Heart Association (NYHA), respectively. Generally, patients in the early stages (A and B) or with lower NYHA classes (I and II) have a better prognosis than those in the later stages (C and D) or higher NYHA classes (III and IV).
Age and Comorbidities: Older patients and those with other chronic conditions, such as diabetes, kidney disease, or chronic obstructive pulmonary disease (COPD), may have a reduced life expectancy compared to younger, otherwise healthy individuals.
Adherence to Treatment: Compliance with prescribed medications, lifestyle modifications, and regular follow-up with healthcare providers can significantly impact the prognosis. Patients who manage their condition effectively may live longer and enjoy a better quality of life.
On average, about 50% of people diagnosed with heart failure live beyond five years. With advances in treatment, many patients can manage their symptoms and maintain a relatively normal life for many years.
Can heart failure be cured?
Currently, there is no cure for heart failure. However, heart failure can be managed effectively with a combination of medical treatments, lifestyle changes, and, in some cases, surgical interventions. The goals of treatment are to alleviate symptoms, improve quality of life, and slow the progression of the disease.
Medical Management: Medications such as ACE inhibitors, beta-blockers, diuretics, and aldosterone antagonists are commonly used to manage heart failure. These drugs help reduce symptoms, prevent hospitalizations, and improve survival.
Lifestyle Changes: Patients are advised to adopt heart-healthy lifestyle practices, including a low-sodium diet, regular physical activity, weight management, and avoiding smoking and excessive alcohol consumption.
Surgical Interventions: In some cases, surgical procedures such as coronary artery bypass grafting (CABG), valve repair or replacement, or the implantation of devices like pacemakers or defibrillators may be necessary to manage heart failure.