Heart failure is a chronic condition where the heart is unable to pump sufficient blood to meet the body’s needs. Managing heart failure requires a comprehensive approach, including medication, lifestyle changes, and often, exercise. This article explores how exercise helps treat heart failure and offers insights into its benefits, safety considerations, and recommended types of physical activity for patients.
Understanding Heart Failure
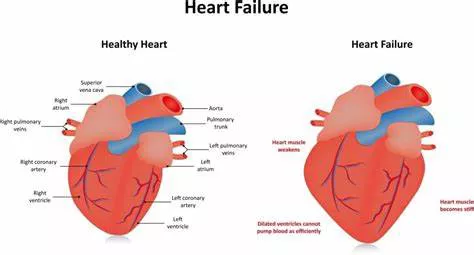
Heart failure, also known as congestive heart failure, can result from various underlying conditions such as coronary artery disease, high blood pressure, or previous heart attacks. Symptoms often include shortness of breath, fatigue, swollen legs, and rapid heartbeat. While heart failure is a serious condition, advances in treatment have significantly improved patient outcomes. One of the key components of managing heart failure is regular exercise.
How Does Exercise Help Heart Failure?
Improving Cardiovascular Health
Exercise strengthens the heart muscle, enabling it to pump blood more efficiently. This improved efficiency means the heart doesn’t have to work as hard to deliver blood throughout the body. Regular aerobic exercise, such as walking or cycling, can enhance the heart’s pumping ability, reduce symptoms of heart failure, and improve overall cardiovascular health.
Enhancing Blood Flow
Physical activity promotes better circulation, which can help reduce the buildup of fluid in the legs and lungs—a common symptom in heart failure patients. Improved blood flow can also lead to better oxygenation of tissues, reducing fatigue and enhancing energy levels.
Reducing Blood Pressure
High blood pressure is a significant risk factor for heart failure. Exercise helps lower blood pressure by improving the elasticity of blood vessels, reducing the workload on the heart. Over time, regular physical activity can lead to sustained reductions in blood pressure, contributing to better heart health.
Managing Weight
Obesity exacerbates heart failure by putting additional strain on the heart. Exercise, combined with a healthy diet, helps in weight management. Losing excess weight reduces the burden on the heart, lowers blood pressure, and improves lipid profiles, which collectively enhance heart function and overall health.
Improving Muscle Strength and Endurance
Heart failure often leads to muscle weakness and decreased physical stamina. Exercise helps counteract these effects by improving muscle strength and endurance. Stronger muscles are more efficient at using oxygen, which can reduce the heart’s workload during physical activity and everyday tasks.
Enhancing Mental Health
Living with heart failure can take a toll on mental health, leading to anxiety and depression. Exercise is known to release endorphins, which are natural mood lifters. Regular physical activity can improve mental well-being, reduce stress levels, and enhance the quality of life for heart failure patients.
Safety Considerations for Exercising with Heart Failure
Consultation with Healthcare Providers
Before starting any exercise program, it is crucial for heart failure patients to consult their healthcare providers. Physicians can assess the patient’s condition, recommend appropriate types and intensities of exercise, and monitor progress.
Personalized exercise plans ensure that patients engage in activities that are safe and beneficial for their specific health status.
Monitoring Symptoms
Patients should be educated on how to monitor their symptoms during exercise. Warning signs such as:
- unusual shortness of breath
- chest pain
- dizziness
- palpitations
Should prompt immediate cessation of activity and consultation with a healthcare provider. Keeping a symptom diary can help track progress and identify any potential issues early.
Gradual Progression
Starting slowly and gradually increasing the intensity and duration of exercise is essential for heart failure patients. A typical recommendation is to begin with low-intensity activities such as walking, and slowly build up to more moderate-intensity exercises as tolerated. This approach helps prevent overexertion and allows the heart and body to adapt gradually to increased physical demands.
Warm-Up and Cool-Down
Incorporating warm-up and cool-down periods into exercise routines is important to prepare the body for physical activity and to prevent injury. Warm-ups can include gentle stretching and light aerobic activity, while cool-downs should involve a gradual reduction in exercise intensity followed by stretching.
Recommended Types of Exercise for Heart Failure Patients
Aerobic Exercise
Aerobic exercises are particularly beneficial for heart failure patients as they improve cardiovascular fitness and enhance the heart’s ability to pump blood. Recommended aerobic activities include:
Walking: A low-impact, easily accessible form of exercise that can be done anywhere.
Cycling: Stationary or outdoor cycling can be a good way to improve leg strength and cardiovascular health.
Swimming: Offers a full-body workout and is gentle on the joints, making it suitable for those with joint pain or arthritis.
Dancing: A fun way to engage in physical activity that also provides cardiovascular benefits.
Resistance Training
Resistance training, or strength training, helps build muscle mass and strength. For heart failure patients, light to moderate resistance training can improve overall muscle function and endurance. Examples include:
Weightlifting: Using light weights or resistance bands.
Bodyweight Exercises: Such as squats, lunges, and push-ups.
Flexibility And Balance Exercises
Improving flexibility and balance can reduce the risk of falls and enhance overall mobility. Activities such as yoga and tai chi are excellent for heart failure patients, as they combine gentle stretching with balance exercises.
Interval Training
For some patients, supervised interval training can be beneficial. This involves alternating short bursts of intense activity with periods of rest or low-intensity exercise. Interval training can improve cardiovascular fitness more efficiently in a shorter amount of time, but it should only be done under medical supervision.
Conclusion
Exercise is a powerful tool in the management of heart failure. It offers numerous benefits, including improved cardiovascular health, enhanced blood flow, reduced blood pressure, weight management, increased muscle strength, and better mental health. However, it is essential for heart failure patients to approach exercise with caution, consulting healthcare providers, monitoring symptoms, and progressing gradually.
By incorporating aerobic, resistance, flexibility, and balance exercises into their routines, patients can significantly improve their quality of life and manage heart failure more effectively. Regular physical activity, tailored to individual capabilities and preferences, can transform the treatment landscape for heart failure, offering hope and improved health outcomes for those living with this chronic condition.
FAQs
How Long Can an Elderly Person Live with Heart Failure?
The life expectancy of an elderly person with heart failure varies significantly based on several factors, including the severity of the condition, the presence of other health issues, how well the condition is managed, and the individual’s overall health. Generally, heart failure is a progressive condition, and its impact on life expectancy can be significant.
Severity of Heart Failure: The New York Heart Association (NYHA) classifies heart failure into four classes, with Class I being the least severe and Class IV being the most severe. Life expectancy tends to be longer in the earlier stages (Class I and II) and shorter in the advanced stages (Class III and IV).
Management and Treatment: Proper management of heart failure through medications, lifestyle changes, and regular medical check-ups can significantly improve life expectancy. Treatments such as beta-blockers, ACE inhibitors, and lifestyle changes like diet and exercise can help control symptoms and slow progression.
Age and General Health: Older patients with heart failure may have a shorter life expectancy due to the natural aging process and potential frailty. However, individual health status plays a critical role; some elderly patients with good general health may live many years with heart failure.
On average, studies suggest that about 50% of people diagnosed with heart failure live beyond five years. However, many factors influence this statistic, and some individuals live much longer with appropriate care and management.
What Can I Eat If I Have Heart Failure?
Diet plays a crucial role in managing heart failure. The goal is to reduce the workload on the heart, manage symptoms, and improve overall health. Here are some dietary recommendations:
1. Limit Sodium Intake:
Excess sodium can cause fluid retention, making it harder for the heart to pump. Aim to consume less than 2,300 milligrams of sodium per day, and ideally closer to 1,500 milligrams.
Avoid: Processed foods, canned soups, salty snacks, and fast food.
Choose: Fresh fruits and vegetables, low-sodium products, and herbs and spices for seasoning instead of salt.
2. Eat a Balanced Diet:
A heart-healthy diet should include a variety of nutrients from different food groups.
Fruits and Vegetables: Aim for at least 5 servings per day. They are rich in vitamins, minerals, and fiber, and low in calories.
Whole Grains: Include whole grains such as brown rice, quinoa, and whole wheat bread. These are high in fiber and nutrients.
Lean Proteins: Choose lean meats, poultry, fish, beans, and legumes.
Fish high in omega-3 fatty acids, like salmon and mackerel, are particularly beneficial.
Healthy Fats: Opt for unsaturated fats found in nuts, seeds, avocados, and olive oil. Avoid trans fats and limit saturated fats.
3. Manage Fluid Intake:
Some heart failure patients need to monitor their fluid intake to prevent fluid overload.
Discuss with your doctor to determine how much fluid you should consume daily.
Limit high-fluid foods such as soups and gelatin if advised by your healthcare provider.
4. Limit Alcohol and Caffeine:
Alcohol can weaken the heart muscle, and caffeine can cause palpitations.
Follow your doctor’s advice regarding alcohol and caffeine consumption.
Limit to moderate levels if permitted, such as one drink per day for women and two for men.
What Are the Levels of Heart Failure?
Class I: No limitation of physical activity. Ordinary physical activity does not cause undue fatigue, palpitation, or shortness of breath.
Class II: Slight limitation of physical activity. Comfortable at rest, but ordinary physical activity results in fatigue, palpitation, or shortness of breath.
Class III: Marked limitation of physical activity. Comfortable at rest, but less than ordinary activity causes fatigue, palpitation, or shortness of breath.
Class IV: Unable to carry out any physical activity without discomfort. Symptoms of heart failure are present even at rest, and any physical activity increases discomfort.
ACC/AHA Stages of Heart Failure:
Stage A: High risk for developing heart failure but no structural heart disease or symptoms. Risk factors include hypertension, diabetes, obesity, and coronary artery disease.
Stage B: Structural heart disease is present, but no symptoms of heart failure. This stage includes individuals with a previous heart attack or valve disease.
Stage C: Structural heart disease with prior or current symptoms of heart failure. Symptoms include fatigue, shortness of breath, and reduced exercise tolerance.
Stage D: Advanced heart failure with symptoms at rest despite maximal medical therapy. This stage may require specialized interventions such as mechanical circulatory support, heart transplant, or palliative care.