Right-sided heart failure, also known as right ventricular failure, occurs when the right ventricle of the heart is unable to pump blood effectively to the lungs. This condition can lead to a range of symptoms and complications that affect various parts of the body. Understanding the signs and symptoms of right-sided heart failure is crucial for early diagnosis and treatment.
Introduction to Right-Sided Heart Failure
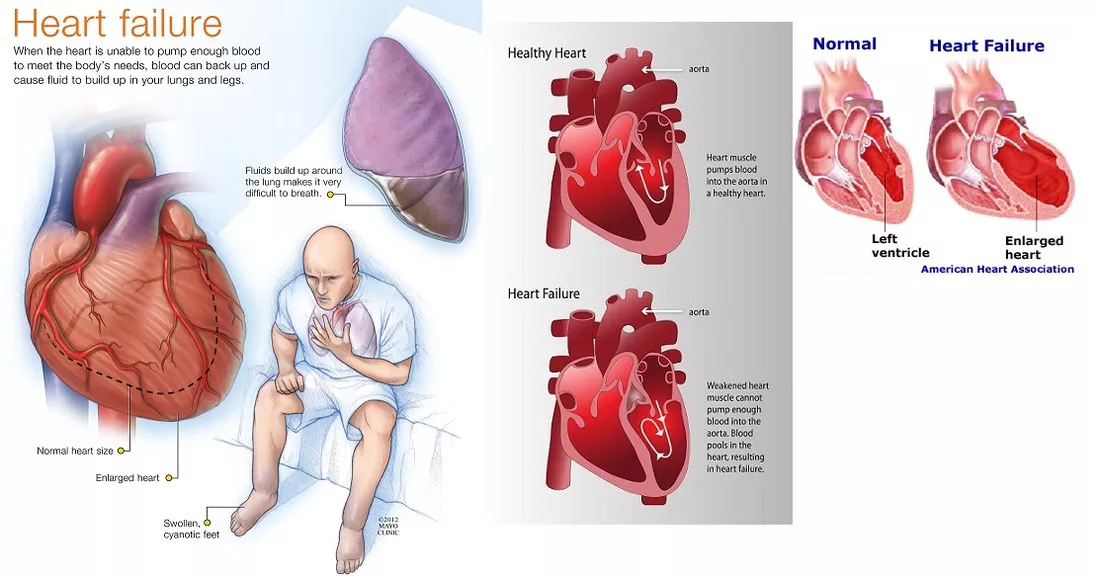
Right-sided heart failure is a condition where the right side of the heart loses its ability to pump blood efficiently. The right ventricle is responsible for pumping blood to the lungs, where it is oxygenated before being sent to the rest of the body.
When the right ventricle fails, blood backs up into the veins, causing a range of symptoms primarily associated with fluid retention and congestion.
Common Causes of Right-Sided Heart Failure
Several factors can contribute to the development of right-sided heart failure. Some of the most common causes include:
Left-sided heart failure: Often, right-sided heart failure is a consequence of left-sided heart failure. When the left side of the heart fails, increased pressure is transferred back through the lungs to the right side of the heart, leading to right ventricular failure.
Chronic lung diseases: Conditions such as chronic obstructive pulmonary disease (COPD) and pulmonary hypertension can increase the workload on the right ventricle, eventually leading to its failure.
Congenital heart defects: Some individuals are born with heart defects that can predispose them to right-sided heart failure.
Pulmonary embolism: A blood clot in the lungs can acutely strain the right side of the heart, potentially leading to right-sided heart failure.
Signs of Right-Sided Heart Failure
Peripheral Edema
One of the hallmark signs of right-sided heart failure is peripheral edema, which is the swelling of the lower extremities.
This occurs because blood backs up in the veins, leading to increased pressure and fluid leakage into the surrounding tissues. Patients may notice swelling in their ankles, feet, and legs. In severe cases, edema can extend to the thighs and abdomen.
Abdominal Swelling and Ascites
In addition to peripheral edema, patients with right-sided heart failure may experience abdominal swelling, known as ascites. This is caused by the accumulation of fluid in the abdominal cavity. Ascites can lead to discomfort, a feeling of fullness, and difficulty breathing when lying down.
Jugular Venous Distension
Jugular venous distension (JVD) is another significant sign of right-sided heart failure. It occurs when the jugular veins in the neck become visibly swollen due to increased pressure from blood backing up in the venous system. JVD is often assessed by healthcare providers as a clinical indicator of right-sided heart failure.
Hepatomegaly
Hepatomegaly, or an enlarged liver, is a common manifestation of right-sided heart failure. The liver becomes congested with blood, leading to swelling and tenderness. Patients may experience right upper quadrant abdominal pain and a sensation of fullness.
Gastrointestinal Symptoms
Right-sided heart failure can also cause various gastrointestinal symptoms due to congestion of the gastrointestinal tract.
These symptoms include nausea, loss of appetite, and bloating. Patients may experience early satiety, where they feel full after eating only small amounts of food.
Fatigue and Weakness
Fatigue and weakness are common symptoms of heart failure in general, including right-sided heart failure. Reduced cardiac output and poor circulation lead to decreased oxygen delivery to the muscles and tissues, resulting in generalized fatigue and a lack of energy.
Cyanosis
Cyanosis, a bluish discoloration of the skin and mucous membranes, can occur in advanced cases of right-sided heart failure. It is a sign of inadequate oxygenation of the blood. Cyanosis is often observed in the lips, fingertips, and toes.
Shortness of Breath
Although shortness of breath is more commonly associated with left-sided heart failure, it can also be a symptom of right-sided heart failure, particularly when pulmonary hypertension or lung disease is present. Patients may experience difficulty breathing during physical activity or when lying flat.
Weight Gain
Rapid weight gain due to fluid retention is another indicator of right-sided heart failure. Patients may notice an increase in body weight over a short period, often accompanied by swelling in various parts of the body.
Nocturia
Nocturia, or frequent urination at night, is a symptom associated with fluid redistribution in right-sided heart failure. When a person lies down, fluid that has accumulated in the lower extremities during the day returns to the bloodstream and is filtered by the kidneys, leading to increased urine production at night.
Diagnosing
Right-Sided Heart Failure
Diagnosing right-sided heart failure involves a combination of clinical evaluation, imaging studies, and laboratory tests.
Healthcare providers will typically perform a physical examination, looking for signs such as JVD, peripheral edema, and hepatomegaly. They may also order the following tests:
Echocardiogram: This imaging test uses ultrasound to evaluate the structure and function of the heart. It can help identify right ventricular dysfunction and measure the pressure in the pulmonary arteries.
Chest X-ray: A chest X-ray can reveal signs of fluid accumulation in the lungs and enlargement of the heart.
Electrocardiogram (ECG): An ECG records the electrical activity of the heart and can detect abnormalities in heart rhythm and signs of strain on the right ventricle.
Blood tests: Blood tests, including B-type natriuretic peptide (BNP) levels, can help assess the severity of heart failure and guide treatment decisions.
Treatment of Right-Sided Heart Failure
The treatment of right-sided heart failure aims to relieve symptoms, improve quality of life, and address the underlying causes.
Management strategies may include:
Medications: Diuretics are commonly prescribed to reduce fluid retention and relieve symptoms such as edema and ascites.
Other medications, such as ACE inhibitors, beta-blockers, and aldosterone antagonists, may be used to manage heart failure and improve heart function.
Lifestyle modifications: Patients are often advised to make lifestyle changes, such as reducing salt intake, maintaining a healthy weight, and engaging in regular physical activity. These changes can help manage symptoms and prevent further deterioration of heart function.
Oxygen therapy: For patients with low blood oxygen levels, supplemental oxygen may be prescribed to improve oxygenation and reduce symptoms of shortness of breath and fatigue.
Treatment of underlying conditions: Addressing the root cause of right-sided heart failure is crucial. This may involve treating lung diseases, managing pulmonary hypertension, or repairing congenital heart defects.
Conclusion
Right-sided heart failure is a complex condition with a range of symptoms primarily related to fluid retention and congestion. Recognizing the signs of right-sided heart failure, such as peripheral edema, abdominal swelling, jugular venous distension, and hepatomegaly, is essential for early diagnosis and treatment. Effective management, including medications, lifestyle changes, and addressing underlying conditions, can significantly improve the quality of life for patients with right-sided heart failure. Early intervention and ongoing care are key to preventing complications and optimizing outcomes for those affected by this condition.