Congestive heart failure (CHF) is a chronic condition where the heart struggles to pump blood efficiently, leading to a buildup of fluid in the lungs, liver, abdomen, and lower extremities. CHF can result from various underlying health issues, including coronary artery disease, high blood pressure, and diabetes. While CHF is a serious and progressive disease, advancements in medical science offer a range of treatments to manage symptoms, slow disease progression, and improve the quality of life for patients.
What Is Congestive Heart Failure?
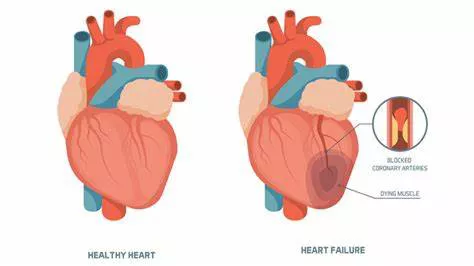
Before delving into the treatments, it’s essential to understand what congestive heart failure is and how it affects the body. CHF occurs when the heart’s pumping ability is weakened, causing blood to move through the heart and body at a slower rate, and pressure in the heart increases. Consequently, the heart can’t pump enough oxygen and nutrients to meet the body’s needs. The chambers of the heart may respond by stretching to hold more blood or by becoming stiff and thickened, which helps keep the blood moving temporarily.
Diagnosing Congestive Heart Failure
Diagnosis of CHF involves a thorough medical history, a physical exam, and various diagnostic tests. These tests may include:
Echocardiogram: Uses sound waves to produce images of the heart, showing its size, structure, and motion.
Electrocardiogram (ECG): Records the electrical activity of the heart and can detect abnormalities.
Chest X-ray: Can reveal the size of the heart and the presence of fluid in the lungs.
Blood tests: Assess kidney function, thyroid function, and check for anemia and other conditions that might affect the heart.
Stress tests: Evaluate how the heart performs under physical stress.
Cardiac MRI: Provides detailed images of the heart’s structure and function.
BNP blood test: Measures the level of B-type natriuretic peptide, which is elevated in heart failure.
Treatment Options for Congestive Heart Failure
The treatment of CHF focuses on managing symptoms, improving quality of life, and slowing disease progression.
Treatment plans are typically tailored to the individual’s condition and may include lifestyle changes, medications, medical devices, and surgical interventions.
Lifestyle Changes
Lifestyle modifications are foundational in managing CHF. They can help reduce symptoms, improve heart function, and enhance overall well-being. Key lifestyle changes include:
Diet: A heart-healthy diet is crucial. This includes reducing sodium intake to prevent fluid retention, eating plenty of fruits and vegetables, whole grains, lean proteins, and avoiding processed foods.
Exercise: Regular physical activity helps strengthen the heart and improve circulation. A tailored exercise program should be developed in consultation with a healthcare provider.
Weight Management: Maintaining a healthy weight reduces the heart’s workload.
Smoking Cessation: Smoking damages blood vessels, raises blood pressure, and reduces oxygen in the blood, exacerbating CHF.
Alcohol Limitation: Excessive alcohol intake can weaken the heart muscle and worsen heart failure.
Monitoring: Regular monitoring of weight, blood pressure, and symptoms can help manage CHF effectively.
Medications
Medications play a pivotal role in the treatment of CHF. They help improve heart function, manage symptoms, and prevent complications. Commonly prescribed medications include:
ACE Inhibitors: These drugs, such as enalapril and lisinopril, help relax blood vessels, lower blood pressure, and reduce the heart’s workload.
Beta-Blockers: Medications like metoprolol and carvedilol slow the heart rate, reduce blood pressure, and decrease the heart’s demand for oxygen.
Diuretics: Often referred to as “water pills,” diuretics like furosemide help reduce fluid buildup in the body.
Aldosterone Antagonists: Spironolactone and eplerenone help remove excess sodium and fluid while retaining potassium.
Angiotensin II Receptor Blockers (ARBs): Drugs like losartan and valsartan relax blood vessels and lower blood pressure.
Digoxin: This medication increases the strength of the heart’s contractions and slows the heart rate.
Vasodilators: Medications such as hydralazine and nitrates help relax blood vessels and reduce the heart’s workload.
Medical Devices
In some cases, medical devices are necessary to manage CHF, particularly in patients with severe symptoms or specific heart function issues. These devices can help improve heart function and manage symptoms.
Implantable Cardioverter-Defibrillator (ICD): This device monitors the heart’s rhythm and delivers electric shocks to restore normal rhythm if a life-threatening arrhythmia occurs.
Cardiac Resynchronization Therapy (CRT): Also known as biventricular pacing, CRT uses a pacemaker to coordinate the contractions of the heart’s ventricles, improving the efficiency of the heart’s pumping action.
Ventricular Assist Devices (VADs): These mechanical pumps are implanted in the chest to help the heart pump blood.
They are often used as a bridge to heart transplantation or as long-term therapy in patients who are not candidates for transplantation.
Emerging Treatments And Therapies
Research in heart failure treatment is ongoing, and several emerging therapies show promise in improving outcomes for patients with CHF.
Gene Therapy: Investigating ways to repair or replace faulty genes that contribute to heart failure.
Stem Cell Therapy: Exploring the potential of stem cells to regenerate damaged heart tissue.
New Medications: Developing drugs that target specific pathways involved in heart failure, such as neprilysin inhibitors and SGLT2 inhibitors.
Palliative Care And Support
Palliative care focuses on providing relief from the symptoms and stress of CHF, improving the quality of life for patients and their families. It can be provided alongside curative treatments or as part of end-of-life care. Palliative care teams work to manage pain, provide emotional support, and assist with decision-making regarding treatment options.
Living with Congestive Heart Failure
Living with CHF requires ongoing management and regular communication with healthcare providers. Patients should adhere to their treatment plans, attend regular check-ups, and report any changes in symptoms promptly. Support from family, friends, and patient support groups can also play a vital role in managing the emotional and psychological aspects of living with CHF.
Conclusion
While congestive heart failure is a serious and chronic condition, a variety of treatments are available to manage symptoms, slow disease progression, and improve the quality of life. From lifestyle changes and medications to medical devices and surgical interventions, each patient’s treatment plan is tailored to their specific needs and condition. Ongoing research continues to explore new therapies, offering hope for even better management and outcomes in the future.
FAQs
Can Heart Failure Cause Edema?
Yes, heart failure can cause edema. Edema, or swelling, occurs when excess fluid accumulates in the tissues of the body. In the context of heart failure, this typically happens because the heart is unable to pump blood efficiently, leading to a buildup of pressure in the veins. This pressure forces fluid out of the blood vessels and into the surrounding tissues.
Mechanism of Edema in Heart Failure
Reduced Cardiac Output: Heart failure reduces the heart’s ability to pump blood effectively, leading to decreased blood flow to the kidneys.
Kidney Response: In response, the kidneys retain more sodium and water to increase blood volume and pressure.
Fluid Retention: The retained fluid increases the volume of blood, but the weakened heart struggles to pump this extra volume, causing fluid to leak into tissues.
Venous Pressure: Elevated pressure in the veins, particularly in the legs and ankles, leads to the characteristic swelling seen in heart failure patients.
Symptoms and Areas Affected
Peripheral Edema: Commonly seen in the legs, ankles, and feet.
Pulmonary Edema: Fluid accumulation in the lungs, leading to shortness of breath and difficulty breathing.
Abdominal Edema (Ascites): Swelling in the abdominal area due to fluid accumulation.
What Can I Eat If I Have Heart Failure?
Diet plays a crucial role in managing heart failure. The primary goals are to reduce fluid retention, control blood pressure, and maintain heart health. Here are dietary recommendations for individuals with heart failure:
Sodium Restriction
Limit Sodium Intake: Aim to consume less than 2,000 mg of sodium per day.
Avoid Processed Foods: Processed foods are often high in sodium. Opt for fresh or frozen fruits and vegetables.
Read Labels: Check food labels for sodium content and choose low-sodium options.
Cook at Home: Preparing meals at home allows better control over sodium levels.
Fluid Management
Monitor Fluid Intake: Depending on your condition, your doctor may recommend limiting fluid intake to prevent fluid overload.
Avoid High-Sodium Beverages: Such as sports drinks and sodas.
Nutrient-Rich Foods
Fruits and Vegetables: Rich in vitamins, minerals, and antioxidants. Aim for a variety of colors to ensure a range of nutrients.
Whole Grains: Such as brown rice, oats, and whole wheat products, which provide fiber and essential nutrients.
Lean Proteins: Include sources like chicken, turkey, fish, beans, and legumes. Avoid high-fat meats and processed proteins.
Healthy Fats: Incorporate sources of unsaturated fats like olive oil, avocados, nuts, and seeds.
Heart-Healthy Choices
Limit Saturated and Trans Fats: Found in fatty cuts of meat, full-fat dairy products, and many processed foods. These can raise cholesterol levels and increase heart disease risk.
Choose Low-Fat Dairy: Opt for skim or low-fat milk, yogurt, and cheese.
Moderate Alcohol Consumption: If permitted by your doctor, limit to no more than one drink per day for women and two drinks per day for men.