Coronary artery disease (CAD) is one of the leading causes of morbidity and mortality worldwide. It occurs when the coronary arteries, which supply blood to the heart muscle, become narrowed or blocked. This condition can lead to chest pain (angina), heart attacks, heart failure, and even sudden death. Understanding how someone gets coronary artery disease involves examining a complex interplay of risk factors, lifestyle choices, and underlying health conditions.
The Pathogenesis of Coronary Artery Disease
Atherosclerosis: The Underlying Mechanism
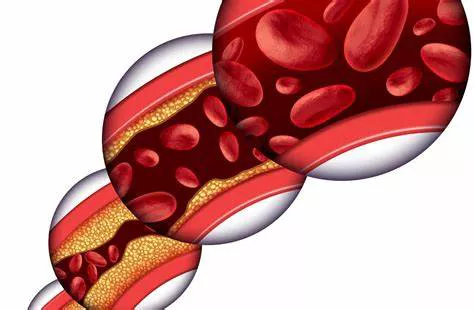
At the core of coronary artery disease is atherosclerosis, a condition characterized by the buildup of fatty deposits (plaques) on the inner walls of the arteries. These plaques are composed of cholesterol, fatty substances, cellular waste products, calcium, and fibrin (a clotting material in the blood). Over time, these deposits can harden and narrow the arteries, restricting blood flow to the heart muscle.
Atherosclerosis begins with damage to the endothelium, the thin layer of cells lining the arteries. This damage can be caused by various factors such as high blood pressure, smoking, diabetes, and high cholesterol levels. Once the endothelium is damaged, cholesterol molecules penetrate the arterial wall, leading to the formation of plaques.
Plaque Development And Progression
The development of atherosclerotic plaques involves several stages:
Fatty Streak Formation: The initial phase involves the accumulation of low-density lipoprotein (LDL) cholesterol within the arterial wall. Macrophages, a type of white blood cell, ingest the LDL cholesterol, transforming into foam cells and creating fatty streaks.
Plaque Growth: As more cholesterol and cells gather, the fatty streak evolves into a more complex structure called a fibrous plaque. This plaque consists of a core of lipid and cellular debris, covered by a fibrous cap made of smooth muscle cells and collagen.
Plaque Rupture: Advanced plaques can become unstable and rupture, exposing the lipid core to the bloodstream. This exposure triggers the formation of a blood clot (thrombus) at the site of the rupture. If the clot significantly blocks the coronary artery, it can result in a heart attack.
Risk Factors for Coronary Artery Disease
Non-Modifiable Risk Factors
Age: The risk of developing coronary artery disease increases with age. Men aged 45 and older and women aged 55 and older are at higher risk.
Gender: Men are generally at greater risk of coronary artery disease than pre-menopausal women. However, after menopause, the risk for women increases and eventually equals that of men.
Family History: A family history of heart disease is a significant risk factor. If a first-degree relative (parent, sibling, or child) has had CAD, particularly at a young age, the risk is higher.
Genetics: Certain genetic predispositions can increase the likelihood of developing CAD. These genetic factors can influence cholesterol metabolism, blood pressure regulation, and inflammatory responses.
Modifiable Risk Factors
High Blood Pressure (Hypertension): Chronic high blood pressure can damage the endothelium and accelerate the process of atherosclerosis. Managing blood pressure through lifestyle changes and medications can reduce the risk.
High Cholesterol Levels: Elevated levels of LDL cholesterol contribute to plaque formation. Conversely, high-density lipoprotein (HDL) cholesterol helps remove cholesterol from the bloodstream. A healthy diet, exercise, and medications can help maintain optimal cholesterol levels.
Smoking: Smoking damages the endothelium, promotes plaque buildup, and reduces oxygen supply to the heart. Quitting smoking significantly lowers the risk of CAD.
Diabetes: Diabetes increases the risk of coronary artery disease by promoting inflammation, increasing cholesterol levels, and damaging blood vessels. Controlling blood sugar levels is crucial in reducing this risk.
Obesity: Excess body weight, particularly around the abdomen, is associated with high blood pressure, high cholesterol, and diabetes, all of which contribute to CAD. Weight loss through diet and exercise can improve heart health.
Physical Inactivity: Lack of regular physical activity contributes to weight gain, high blood pressure, and cholesterol problems. Regular exercise strengthens the heart and improves circulation.
Unhealthy Diet: Diets high in saturated fats, trans fats, cholesterol, and sodium can increase the risk of CAD. A heart-healthy diet includes plenty of fruits, vegetables, whole grains, lean proteins, and healthy fats.
Excessive Alcohol Consumption: While moderate alcohol consumption may have some protective effects on the heart, excessive drinking can lead to high blood pressure, heart failure, and other health issues. Moderation is key.
Emerging Risk Factors
Inflammation: Chronic inflammation is now recognized as a critical factor in the development and progression of atherosclerosis. High levels of C-reactive protein (CRP), a marker of inflammation, have been associated with an increased risk of CAD.
Metabolic Syndrome: This cluster of conditions—including high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels—significantly increases the risk of heart disease.
Stress and Mental Health: Chronic stress, depression, and anxiety can contribute to heart disease. Stress can lead to unhealthy behaviors like smoking and overeating and can directly affect heart health through hormonal changes.
Sleep Apnea: Obstructive sleep apnea, a condition where breathing repeatedly stops and starts during sleep, is associated with high blood pressure, heart rhythm disorders, and CAD.
Preventive Measures And Lifestyle Modifications
Diet and Nutrition
Adopting a heart-healthy diet is crucial in preventing and managing coronary artery disease. Key dietary recommendations include:
Increasing Fiber Intake: Consuming more fruits, vegetables, whole grains, and legumes can help reduce cholesterol levels and improve heart health.
Choosing Healthy Fats: Replace saturated and trans fats with monounsaturated and polyunsaturated fats found in olive oil, nuts, seeds, and fatty fish.
Reducing Sodium: Lowering sodium intake can help manage blood pressure. Avoid processed foods and limit salt added during cooking.
Limiting Sugar: Reduce the consumption of sugary beverages and snacks to prevent obesity and diabetes.
Regular Physical Activity
Engaging in regular physical activity helps maintain a healthy weight, lowers blood pressure, improves cholesterol levels, and strengthens the heart. Aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity exercise per week, along with muscle-strengthening activities on two or more days per week.
Weight Management
Maintaining a healthy weight is essential for reducing the risk of CAD.
Calculate your body mass index (BMI) to determine a healthy weight range and work towards achieving and maintaining it through a balanced diet and regular exercise.
Smoking Cessation
Quitting smoking is one of the most effective ways to reduce the risk of coronary artery disease. Seek support through smoking cessation programs, medications, or counseling to overcome nicotine addiction.
Managing Chronic Conditions
Effectively managing chronic conditions such as hypertension, diabetes, and high cholesterol is crucial in preventing CAD.
Regular check-ups, medications, and lifestyle modifications can help keep these conditions under control.
Stress Reduction
Incorporating stress-reduction techniques such as mindfulness, meditation, yoga, and deep breathing exercises can improve mental health and reduce the risk of heart disease. Maintaining social connections and seeking professional help for mental health issues is also important.
Medical Interventions And Treatments
Medications
Several medications can help manage the risk factors associated with coronary artery disease:
Statins: These drugs lower LDL cholesterol levels and reduce inflammation.
Antihypertensives: Medications such as ACE inhibitors, beta-blockers, and calcium channel blockers help control high blood pressure.
Antidiabetics: These drugs help manage blood sugar levels in people with diabetes.
Antiplatelet Agents: Aspirin and other antiplatelet drugs reduce the risk of blood clots.
Surgical And Non-Surgical Procedures
In advanced cases of CAD, medical procedures may be necessary to restore blood flow to the heart:
Angioplasty and Stenting: A catheter with a balloon is inserted into the narrowed artery. The balloon is inflated to open the artery, and a stent (a small mesh tube) is placed to keep it open.
Coronary Artery Bypass Grafting (CABG): In this surgery, a healthy blood vessel is taken from another part of the body and used to bypass the blocked coronary artery.
Conclusion
Coronary artery disease is a multifactorial condition resulting from a combination of genetic predispositions, lifestyle choices, and underlying health conditions. Understanding the pathogenesis of atherosclerosis and the various risk factors involved is crucial for prevention and management. By adopting a heart-healthy lifestyle, managing chronic conditions, and seeking appropriate medical interventions, individuals can significantly reduce their risk of developing coronary artery disease and improve their overall heart health.