Heart transplantation is a life-saving procedure for patients with end-stage heart disease. While it offers hope and a chance for a new life, many wonder about the long-term survival and quality of life post-transplant. This article delves into the various factors influencing the longevity of heart transplant recipients, the advancements in medical science that have improved outcomes, and the challenges that still exist.
What Is Heart Transplantation?
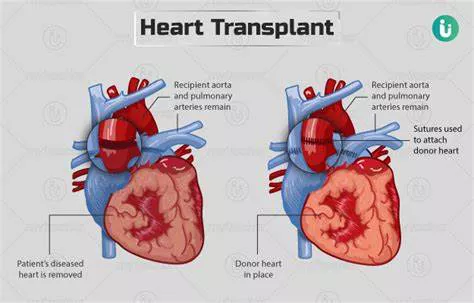
A heart transplant is a surgical procedure where a diseased or failing heart is replaced with a healthier donor heart. This procedure is typically reserved for patients with severe heart failure or other serious heart conditions that do not respond to conventional treatments. The primary goal of a heart transplant is to extend the recipient’s life and improve their quality of life.
Survival Rates And Longevity
Short-Term Survival
The immediate period following a heart transplant is critical. According to data from the International Society for Heart and Lung Transplantation (ISHLT), the one-year survival rate for heart transplant recipients is approximately 85-90%.
This high survival rate can be attributed to improved surgical techniques, better postoperative care, and advanced immunosuppressive therapies.
Long-Term Survival
While short-term survival rates are promising, the focus often shifts to long-term survival. On average, heart transplant recipients can expect to live for about 10-15 years post-transplant. However, many patients live much longer, with some surviving 20 years or more. The median survival time, according to the ISHLT, is around 11 years.
Factors Influencing Longevity
Age: Age plays a significant role in determining the longevity of heart transplant recipients. Younger patients generally have better outcomes compared to older recipients. This is partly due to younger patients having fewer comorbidities and a stronger ability to recover from surgery. Older patients, especially those over 65, may have a reduced life expectancy post-transplant, though many still achieve significant extensions to their lives.
Underlying Health Conditions
Pre-existing health conditions can impact survival rates. Patients with conditions like diabetes, kidney disease, or chronic infections may face more complications post-transplant. Managing these comorbidities effectively is crucial for extending life expectancy.
Donor Heart Quality
The condition of the donor heart also affects the recipient’s longevity.
Donor hearts from younger, healthier individuals tend to result in better outcomes. The matching process, including blood type and size compatibility, is essential for reducing the risk of rejection and complications.
Immunosuppressive Therapy
Immunosuppressive drugs are necessary to prevent the body from rejecting the new heart. However, these medications come with side effects, including an increased risk of infections and certain cancers.
Advances in immunosuppressive therapy have improved long-term survival, but managing these drugs requires a delicate balance.
Post-Transplant Care
Regular follow-up care, including frequent medical check-ups, is vital for monitoring the heart’s function and detecting potential issues early.
Adherence to prescribed medications and lifestyle modifications, such as a healthy diet and regular exercise, significantly influence long-term outcomes.
Advancements in Heart Transplantation
Improved Surgical Techniques
Surgical advancements have played a crucial role in improving survival rates. Minimally invasive techniques and better surgical instruments have reduced the risk of complications during and after the procedure.
Better Immunosuppressive Drugs
The development of more effective immunosuppressive drugs has been a game-changer. Newer medications offer better protection against rejection while minimizing side effects. Research continues to focus on developing drugs that provide optimal immunosuppression with fewer risks.
Innovations in Organ Preservation
Innovations in organ preservation have extended the viability of donor hearts. Techniques like ex vivo perfusion, where the heart is kept functioning outside the body until transplantation, have improved the quality of transplanted organs and increased the success rates of transplants.
Personalized Medicine
Personalized medicine, where treatments are tailored to the individual patient’s genetic makeup, is becoming increasingly important in transplantation. Genetic testing can help determine the best immunosuppressive therapy and predict potential complications, leading to better outcomes.
Challenges And Complications
Organ Rejection
Organ rejection remains a significant challenge despite advancements in immunosuppressive therapy. There are three types of rejection: hyperacute, acute, and chronic. Acute rejection can occur within the first year and is managed with medication adjustments. Chro
nic rejection, however, is a long-term issue that can lead to transplant failure.
Infections
The immunosuppressive drugs necessary to prevent rejection also weaken the immune system, making recipients more susceptible to infections. These infections can be severe and impact long-term survival.
Cancer Risk
Heart transplant recipients have a higher risk of developing certain cancers, particularly skin cancers and lymphomas. This increased risk is due to the long-term use of immunosuppressive drugs.
Cardiac Allograft Vasculopathy (CAV)
CAV is a form of coronary artery disease that affects the transplanted heart. It is a leading cause of long-term transplant failure. Regular monitoring and preventive measures are essential to manage this condition.
Quality of Life Post-Transplant
Physical Health
Most heart transplant recipients experience a significant improvement in their physical health. They can often return to normal activities, including work and exercise. However, they must remain vigilant about their health, adhering to medical advice and attending regular check-ups.
Mental Health
The mental health of transplant recipients is an important aspect of their overall well-being. The stress of undergoing a major surgery, adjusting to a new lifestyle, and the fear of rejection can affect mental health. Support from healthcare providers, family, and mental health professionals is crucial.
Lifestyle Modifications
Adopting a healthy lifestyle is critical for maintaining the health of the transplanted heart. This includes following a heart-healthy diet, engaging in regular physical activity, avoiding smoking, and limiting alcohol consumption.
Conclusion
Heart transplantation has transformed the lives of many patients with end-stage heart disease, offering them a second chance at life. While the procedure comes with challenges, advancements in medical science have significantly improved survival rates and quality of life. On average, heart transplant recipients can expect to live for 10-15 years, with many living longer.
The longevity of a heart transplant recipient depends on various factors, including age, underlying health conditions, donor heart quality, and adherence to post-transplant care. As research and technology continue to advance, the future holds promise for even better outcomes and longer lives for heart transplant recipients.