Blocked heart arteries, medically known as coronary artery disease (CAD), is a common yet serious condition that can lead to significant health problems, including heart attacks and heart failure.
Understanding the symptoms of blocked heart arteries is crucial for early detection and treatment. This article will delve into the various signs and symptoms associated with blocked heart arteries, the underlying mechanisms, risk factors, and the importance of timely medical intervention.
Understanding Blocked Heart Arteries
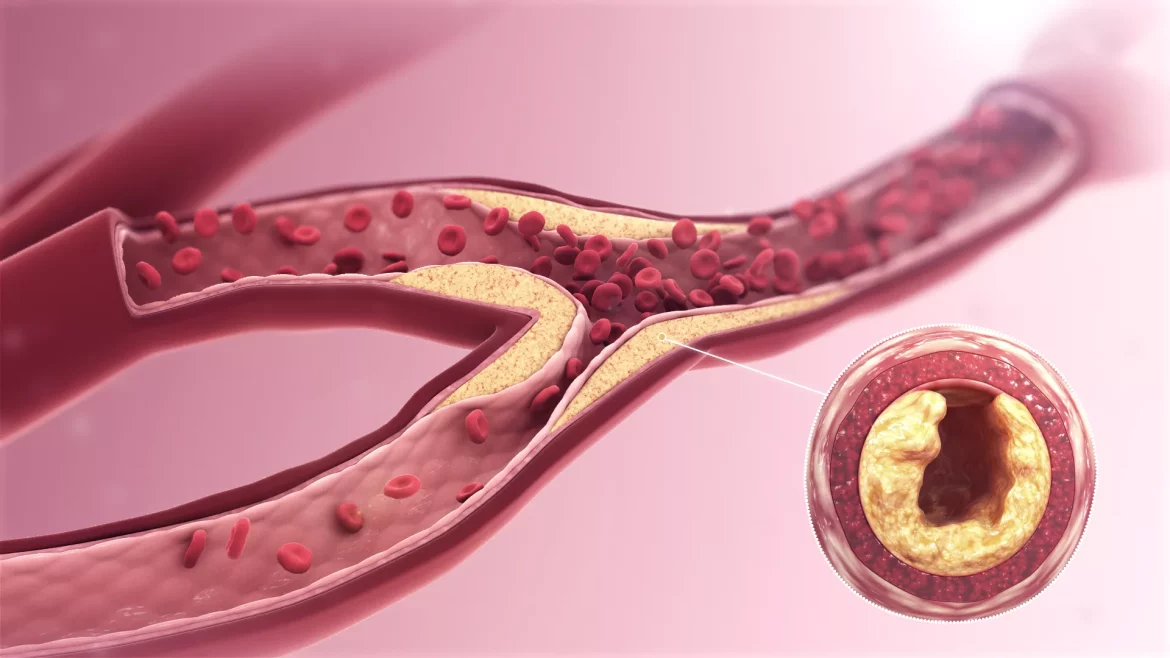
Coronary artery disease occurs when the coronary arteries, which supply oxygen-rich blood to the heart muscle, become narrowed or blocked due to the buildup of fatty deposits called plaques. This process, known as atherosclerosis, can lead to reduced blood flow to the heart, causing a range of symptoms that vary in severity and type.
Key Symptoms of Blocked Heart Arteries
Chest Pain or Discomfort (Angina)
Stable Angina: This type of chest pain occurs predictably with physical exertion or emotional stress and typically subsides with rest or medication. It often feels like pressure, squeezing, fullness, or pain in the center of the chest.
Unstable Angina: This is a more severe form of chest pain that occurs unexpectedly, even at rest. It is a medical emergency as it indicates a higher risk of heart attack.
Shortness of Breath
When the heart is unable to pump enough blood due to blocked arteries, it can lead to shortness of breath, especially during physical activity. This symptom occurs because the body is not receiving adequate oxygen, causing respiratory distress.
Fatigue
Chronic fatigue can be a subtle but significant symptom of blocked heart arteries. Reduced blood flow means the heart has to work harder to pump blood, leading to overall tiredness and weakness.
Palpitations
Patients may experience an abnormal awareness of their heartbeat, which can feel like the heart is racing, fluttering, or skipping beats. This occurs due to irregular heart rhythms caused by reduced blood supply to the heart.
Dizziness or Lightheadedness
Insufficient blood flow to the brain can result in dizziness or a feeling of lightheadedness. In severe cases, it can cause fainting spells, indicating a critical reduction in blood supply.
Nausea and Sweating
Nausea and cold sweats are often overlooked but can be significant indicators of blocked heart arteries. These symptoms are more common during a heart attack and may accompany chest pain.
Pain in Other Parts of the Body
Blocked heart arteries can cause referred pain, where discomfort is felt in areas other than the chest, such as the shoulders, arms (particularly the left arm), neck, jaw, or back.
Mechanisms Behind Symptoms
The symptoms of blocked heart arteries are primarily due to reduced blood flow and oxygen supply to the heart muscle and other vital organs. Here’s a closer look at the mechanisms:
Ischemia: This occurs when blood flow is restricted, leading to insufficient oxygen supply to the heart muscle. Ischemia causes chest pain and can trigger other symptoms like shortness of breath and fatigue.
Infarction: A complete blockage can lead to myocardial infarction, commonly known as a heart attack. This is characterized by severe chest pain, nausea, sweating, and can be life-threatening.
Arrhythmias: Irregular heartbeats or palpitations can result from impaired blood flow affecting the heart’s electrical system.
Reduced Cardiac Output: When the heart cannot pump efficiently, it leads to symptoms like fatigue, dizziness, and shortness of breath due to inadequate blood supply to the body.
Risk Factors for Blocked Heart Arteries
Several risk factors increase the likelihood of developing blocked heart arteries, including:
High Blood Pressure: Elevated blood pressure can damage the arteries, making them more susceptible to plaque buildup.
High Cholesterol: High levels of LDL (bad) cholesterol contribute to plaque formation in the arteries.
Smoking: Tobacco use damages the lining of the arteries and accelerates the process of atherosclerosis.
Diabetes: Diabetes increases the risk of coronary artery disease due to its impact on blood vessels and metabolic functions.
Obesity: Excess body weight strains the heart and contributes to high blood pressure, diabetes, and high cholesterol.
Sedentary Lifestyle: Lack of physical activity is a significant risk factor for heart disease.
Unhealthy Diet: Diets high in saturated fats, trans fats, and cholesterol can lead to plaque buildup in the arteries.
Family History: A family history of heart disease increases the risk of developing blocked heart arteries.
Diagnostic Methods
Healthcare providers use various diagnostic tools to detect blocked heart arteries, including:
Electrocardiogram (ECG or EKG): This test measures the electrical activity of the heart and can detect abnormalities caused by insufficient blood flow.
Stress Testing: Stress tests assess how the heart performs under physical exertion, helping to identify areas with reduced blood flow.
Echocardiogram: This imaging test uses ultrasound to create detailed images of the heart, allowing doctors to see how well it is functioning.
Coronary Angiography: A more invasive procedure where a contrast dye is injected into the coronary arteries, making them visible on X-ray images. This helps to pinpoint the location and severity of blockages.
CT Angiography: This non-invasive test uses CT scans to produce detailed images of the coronary arteries.
Treatment Options
Treatment for blocked heart arteries aims to restore adequate blood flow to the heart. Options include:
Lifestyle Changes: Adopting a heart-healthy lifestyle is crucial. This includes a balanced diet, regular exercise, quitting smoking, and managing stress.
Medications: Various medications can help manage symptoms and prevent further blockages, including:
Antiplatelet Drugs: Such as aspirin, to reduce the risk of blood clots.
Cholesterol-Lowering Drugs: Statins and other medications to lower LDL cholesterol levels.
Beta-Blockers: To reduce heart rate and blood pressure, decreasing the heart’s workload.
ACE Inhibitors: To lower blood pressure and reduce strain on the heart.
Nitrates: To relieve chest pain by dilating the coronary arteries.
Interventional Procedures: When medications are not enough, procedures to restore blood flow might be necessary, such as:
Angioplasty and Stenting: A procedure where a balloon is used to open up blocked arteries, and a stent is placed to keep them open.
Coronary Artery Bypass Grafting (CABG): A surgical procedure where a healthy artery or vein from another part of the body is used to bypass a blocked artery.
Conclusion
Blocked heart arteries are a serious health condition that requires prompt attention and management. By understanding the symptoms, underlying mechanisms, risk factors, and treatment options, individuals can take proactive steps to protect their heart health. Early detection and intervention are key to preventing severe complications and ensuring a better quality of life. If you experience any symptoms of blocked heart arteries, seek medical advice promptly to receive the necessary care and treatment.