Cardiac arrest is a sudden and often fatal medical emergency that occurs when the heart abruptly stops beating. This cessation of heart function halts blood flow to the brain and other vital organs, leading to loss of consciousness and, without immediate intervention, death. Understanding the causes of cardiac arrest is crucial for prevention, timely intervention, and improving survival rates. Various underlying conditions and triggers can lead to cardiac arrest, each with its own mechanisms and risk factors.
Understanding Cardiac Arrest
Cardiac arrest is different from a heart attack, although the two can be related. A heart attack, or myocardial infarction, occurs when blood flow to a part of the heart is blocked, causing heart muscle damage. In contrast, cardiac arrest is an electrical problem where the heart’s rhythm is disrupted, leading to its sudden stop. Both conditions are emergencies, but their causes and treatments can differ significantly.
Primary Causes of Cardiac Arrest
Coronary Artery Disease (CAD):
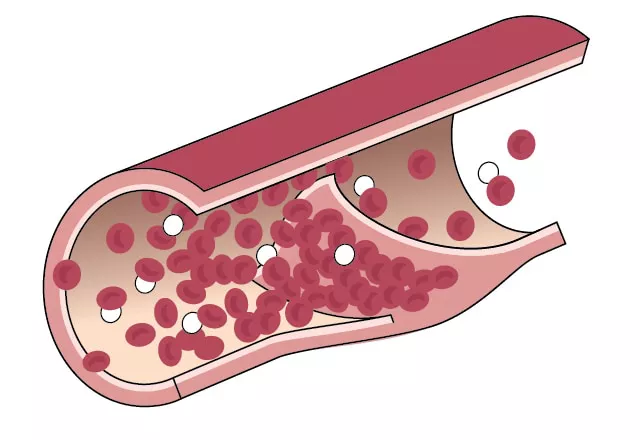
CAD is the most common cause of cardiac arrest. It occurs when the coronary arteries that supply blood to the heart muscle become clogged with fatty deposits (atherosclerosis). This buildup can limit blood flow and oxygen to the heart, leading to ischemia (lack of oxygen) and potentially triggering arrhythmias (irregular heartbeats) that can result in cardiac arrest.
Heart Attack:
A severe heart attack can lead to cardiac arrest. When a heart attack damages a significant portion of the heart muscle, it can disrupt the heart’s electrical system, causing it to stop beating.
Cardiomyopathy:
This refers to diseases of the heart muscle, which can become thickened, enlarged, or stiffened, impairing its ability to pump blood effectively. Various forms of cardiomyopathy, including hypertrophic cardiomyopathy (HCM), dilated cardiomyopathy (DCM), and restrictive cardiomyopathy, can predispose individuals to arrhythmias and cardiac arrest.
Arrhythmias:
Arrhythmias are irregular heartbeats that can be benign or life-threatening. Ventricular fibrillation (VF) and ventricular tachycardia (VT) are two types of arrhythmias that can cause cardiac arrest. VF is a chaotic, disorganized heart rhythm that prevents the heart from pumping effectively, while VT is a fast, regular beating of the ventricles that can deteriorate into VF.
Congenital Heart Disease:
Individuals born with structural heart defects are at higher risk of cardiac arrest. These congenital conditions can lead to abnormal heart rhythms, particularly in children and young adults.
Heart Failure:
Chronic heart failure, where the heart is unable to pump blood efficiently, can increase the risk of cardiac arrest. The weakened heart muscle can be prone to dangerous arrhythmias.
Valvular Heart Disease:
Problems with the heart valves, such as stenosis (narrowing) or regurgitation (leakage), can affect the heart’s function and lead to arrhythmias, increasing the risk of cardiac arrest.
Electrical Abnormalities:
Conditions like Long QT syndrome, Brugada syndrome, and other inherited arrhythmia syndromes involve the heart’s electrical pathways and can cause sudden cardiac arrest, particularly in younger individuals without structural heart disease.
Comorbidities and External Factors:
Other medical conditions, such as severe electrolyte imbalances, extreme physical stress, drug abuse (particularly stimulants), and significant trauma, can also trigger cardiac arrest.
What Causes SCAD Heart?
Spontaneous Coronary Artery Dissection (SCAD) is an uncommon but increasingly recognized cause of acute coronary syndromes, particularly in young women. SCAD occurs when a tear forms in one of the coronary arteries, leading to a separation of the layers within the artery wall. This can create a false lumen where blood accumulates, compressing the true lumen and restricting blood flow to the heart muscle, potentially causing a heart attack and, if severe, cardiac arrest.
SCAD is unique because it often occurs in individuals without the traditional risk factors for coronary artery disease, such as high cholesterol, diabetes, or a history of smoking. The exact cause of SCAD is not fully understood, but several factors may contribute to its development:
Hormonal Changes:
Hormonal fluctuations, particularly during pregnancy or postpartum, have been linked to SCAD. These hormonal changes may weaken the artery walls, making them more susceptible to tears.
Fibromuscular Dysplasia (FMD):
FMD is a condition that causes abnormal cell growth in the walls of medium and large arteries, leading to narrowing, aneurysms, and dissections. Many SCAD patients have been found to have FMD in other arteries, suggesting a possible link.
Connective Tissue Disorders:
Genetic conditions that affect the connective tissues, such as Marfan syndrome and Ehlers-Danlos syndrome, can increase the risk of arterial dissections, including SCAD.
Emotional or Physical Stress:
Intense emotional stress or extreme physical exertion can precipitate SCAD by increasing blood pressure and heart rate, potentially causing a tear in a vulnerable artery.
Inflammatory Conditions:
Autoimmune or inflammatory diseases, such as lupus or inflammatory bowel disease, may contribute to the weakening of the arterial walls, leading to SCAD.
Genetic Factors:
While SCAD is not typically inherited, there may be genetic predispositions that increase susceptibility to arterial dissections.
Recognizing The Symptoms of Cardiac Arrest
Cardiac arrest often occurs suddenly and without warning. However, some individuals may experience warning signs before an arrest, including:
- Chest pain or discomfort
- Shortness of breath
- Palpitations or rapid heartbeats
- Dizziness or lightheadedness
- Unexplained fatigue
During cardiac arrest, the individual will collapse, lose consciousness, and have no pulse or breathing. Immediate intervention with cardiopulmonary resuscitation (CPR) and defibrillation is critical to increase the chances of survival.
Prevention And Risk Reduction
Preventing cardiac arrest involves managing the underlying conditions and risk factors that contribute to heart disease. Key preventive measures include:
Regular Medical Check-ups:
Routine health screenings can help identify and manage risk factors such as high blood pressure, high cholesterol, and diabetes.
Healthy Lifestyle Choices:
A balanced diet, regular exercise, maintaining a healthy weight, and avoiding smoking can reduce the risk of heart disease and cardiac arrest.
Medication Adherence:
For individuals with heart disease or risk factors, adhering to prescribed medications can help control conditions that might lead to cardiac arrest.
Stress Management:
Managing stress through techniques such as mindfulness, relaxation exercises, and counseling can reduce the risk of heart problems.
Awareness and Education:
Educating oneself and others about the signs and symptoms of cardiac arrest and how to perform CPR can save lives in emergency situations.
Conclusion
Cardiac arrest is a life-threatening condition with various causes, ranging from coronary artery disease to rare conditions like SCAD. Understanding these causes, recognizing the symptoms, and taking preventive measures are essential for reducing the incidence and improving outcomes of cardiac arrest. Immediate medical intervention and widespread education on CPR can significantly enhance survival rates, making awareness and preparedness vital components in the fight against cardiac arrest.