Exercise-induced hypertension (EIH) is a condition where blood pressure rises to abnormally high levels during physical activity. This phenomenon can be perplexing, as exercise is typically associated with numerous cardiovascular benefits, including improved blood pressure regulation. However, for some individuals, physical exertion triggers significant increases in blood pressure, potentially leading to adverse health outcomes. Understanding the underlying causes of exercise-induced hypertension is crucial for managing this condition effectively.
Physiological Mechanisms Behind Blood Pressure Regulation
To comprehend what causes exercise-induced hypertension, it’s essential to first understand how blood pressure is regulated during physical activity. Blood pressure is the force exerted by circulating blood on the walls of blood vessels, and it is influenced by several factors, including heart rate, blood volume, and the resistance of blood vessels. During exercise, the body undergoes various physiological changes to meet the increased demand for oxygen and nutrients by the muscles.
Increased Cardiac Output: Exercise prompts the heart to pump more blood to supply the working muscles with oxygen and nutrients. This increase in cardiac output naturally elevates blood pressure.
Vasodilation: To facilitate the increased blood flow, blood vessels, particularly in the muscles, dilate. This vasodilation helps accommodate the higher volume of blood, typically counteracting the rise in blood pressure.
Sympathetic Nervous System Activation: Physical activity stimulates the sympathetic nervous system, which increases heart rate and constricts certain blood vessels, contributing to a rise in blood pressure.
For most individuals, these adjustments result in a moderate increase in blood pressure that is beneficial and well-tolerated. However, in cases of exercise-induced hypertension, these regulatory mechanisms become dysregulated, leading to excessively high blood pressure levels during exercise.
Potential Causes of Exercise-Induced Hypertension
Several factors can contribute to the development of exercise-induced hypertension. These factors can be broadly categorized into physiological, lifestyle-related, and underlying health conditions.
1. Preexisting Hypertension
Individuals with preexisting hypertension are at a higher risk of developing exercise-induced hypertension. When baseline blood pressure is already elevated, the additional increase caused by exercise can push levels into a dangerously high range.
This condition, known as labile hypertension, can result in significant fluctuations in blood pressure during physical activity.
2. Arterial Stiffness
Arterial stiffness is a condition where the arteries become less flexible, making it harder for them to expand and contract with changes in blood flow. This rigidity can result from aging, atherosclerosis, or chronic hypertension. During exercise, the reduced ability of stiff arteries to accommodate increased blood flow can lead to a significant rise in blood pressure.
3. Sympathetic Nervous System Overactivity
The sympathetic nervous system plays a crucial role in regulating cardiovascular responses to exercise. Overactivity of this system can cause excessive vasoconstriction and an increase in heart rate, leading to a disproportionate rise in blood pressure during physical exertion. Factors contributing to sympathetic overactivity include stress, anxiety, and certain medications.
4. Hormonal Imbalances
Hormonal imbalances, particularly involving the renin-angiotensin-aldosterone system (RAAS), can contribute to exercise-induced hypertension. This system regulates blood pressure by controlling blood volume and vascular resistance.
Dysregulation of RAAS can result in inappropriate retention of sodium and water, increasing blood volume and, consequently, blood pressure during exercise.
5. Endothelial Dysfunction
The endothelium is the inner lining of blood vessels, responsible for producing substances that regulate vascular tone and blood flow. Endothelial dysfunction, often associated with conditions like diabetes, obesity, and chronic inflammation, impairs the ability of blood vessels to dilate properly during exercise, leading to increased vascular resistance and elevated blood pressure.
Lifestyle Factors Contributing to Exercise-Induced Hypertension
Apart from physiological and medical conditions, certain lifestyle factors can exacerbate the risk of developing exercise-induced hypertension.
1. High-Sodium Diet
A diet high in sodium can increase blood pressure by causing the body to retain excess fluid, thereby increasing blood volume. This effect can be particularly pronounced during exercise when the body’s demand for blood flow increases.
Reducing sodium intake is a crucial step in managing hypertension and preventing exercise-induced spikes in blood pressure.
2. Sedentary Lifestyle
Lack of regular physical activity can contribute to the development of hypertension and arterial stiffness. When sedentary individuals engage in sudden intense exercise, their cardiovascular system may not be adequately conditioned to handle the increased demand, resulting in a significant rise in blood pressure.
3. Overtraining
While regular exercise is beneficial for cardiovascular health, excessive or overly intense exercise without adequate rest can lead to overtraining syndrome. This condition can cause chronic stress on the cardiovascular system, potentially leading to exercise-induced hypertension. It is essential to balance exercise intensity with sufficient recovery periods.
Underlying Health Conditions And Exercise-Induced Hypertension
Certain underlying health conditions can predispose individuals to exercise-induced hypertension. Addressing these conditions is vital for managing and preventing the condition.
1. Obesity
Obesity is a significant risk factor for hypertension and exercise-induced hypertension. Excess body weight increases the workload on the heart and blood vessels, leading to higher blood pressure levels during exercise. Weight loss through diet and regular physical activity can help mitigate this risk.
2. Diabetes
Diabetes, particularly type 2 diabetes, is often associated with hypertension and endothelial dysfunction. Managing blood sugar levels and maintaining cardiovascular health through medication, diet, and exercise is crucial for individuals with diabetes to prevent exercise-induced hypertension.
3. Kidney Disease
Chronic kidney disease can lead to hypertension due to impaired kidney function and fluid retention. During exercise, individuals with kidney disease may experience exaggerated increases in blood pressure. Managing kidney health through proper treatment and lifestyle modifications is essential for these individuals.
Diagnosis And Monitoring of Exercise-Induced Hypertension
Diagnosing exercise-induced hypertension typically involves measuring blood pressure during and after physical activity.
This can be done using a treadmill or stationary bike test in a controlled environment, where blood pressure is monitored at regular intervals. Ambulatory blood pressure monitoring, which involves wearing a portable device that measures blood pressure throughout the day, can also provide valuable insights into how blood pressure responds to various activities, including exercise.
Management And Treatment Strategies
Managing exercise-induced hypertension requires a multifaceted approach that addresses the underlying causes and incorporates lifestyle modifications, medication, and regular monitoring.
1. Lifestyle Modifications
Diet: Adopting a heart-healthy diet, such as the DASH (Dietary Approaches to Stop Hypertension) diet, can help manage blood pressure. This diet emphasizes fruits, vegetables, whole grains, lean proteins, and low-fat dairy while reducing sodium and unhealthy fats.
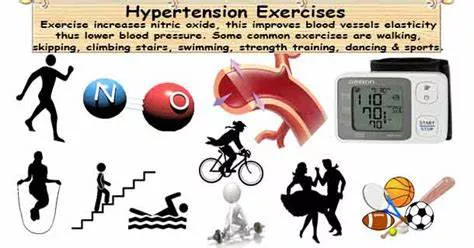
Regular Exercise: Engaging in regular, moderate-intensity exercise can improve cardiovascular fitness and help regulate blood pressure.
Activities such as brisk walking, swimming, and cycling are beneficial.
It is essential to start slowly and gradually increase intensity to avoid sudden spikes in blood pressure.
Weight Management: Achieving and maintaining a healthy weight through diet and exercise can significantly reduce the risk of hypertension and exercise-induced hypertension.
2. Medication
In some cases, medication may be necessary to manage exercise-induced hypertension. Commonly prescribed medications include:
Antihypertensives: Medications such as beta-blockers, ACE inhibitors, and calcium channel blockers can help control blood pressure during exercise.
Diuretics: These medications help reduce blood volume by promoting the excretion of excess fluid and sodium.
It is crucial to work closely with a healthcare provider to determine the most appropriate medication regimen and adjust dosages based on individual responses to exercise.
3. Regular Monitoring
Regular monitoring of blood pressure, both at rest and during exercise, is essential for individuals with exercise-induced hypertension. This can help track progress, evaluate the effectiveness of treatment strategies, and make necessary adjustments.
Conclusion
Exercise-induced hypertension is a complex condition with multiple contributing factors, including physiological mechanisms, lifestyle choices, and underlying health conditions. Understanding what causes exercise-induced hypertension is crucial for effective management and prevention. By adopting a heart-healthy lifestyle, addressing underlying health issues, and working closely with healthcare providers, individuals can manage their blood pressure during exercise and enjoy the numerous benefits of physical activity without compromising their cardiovascular health.