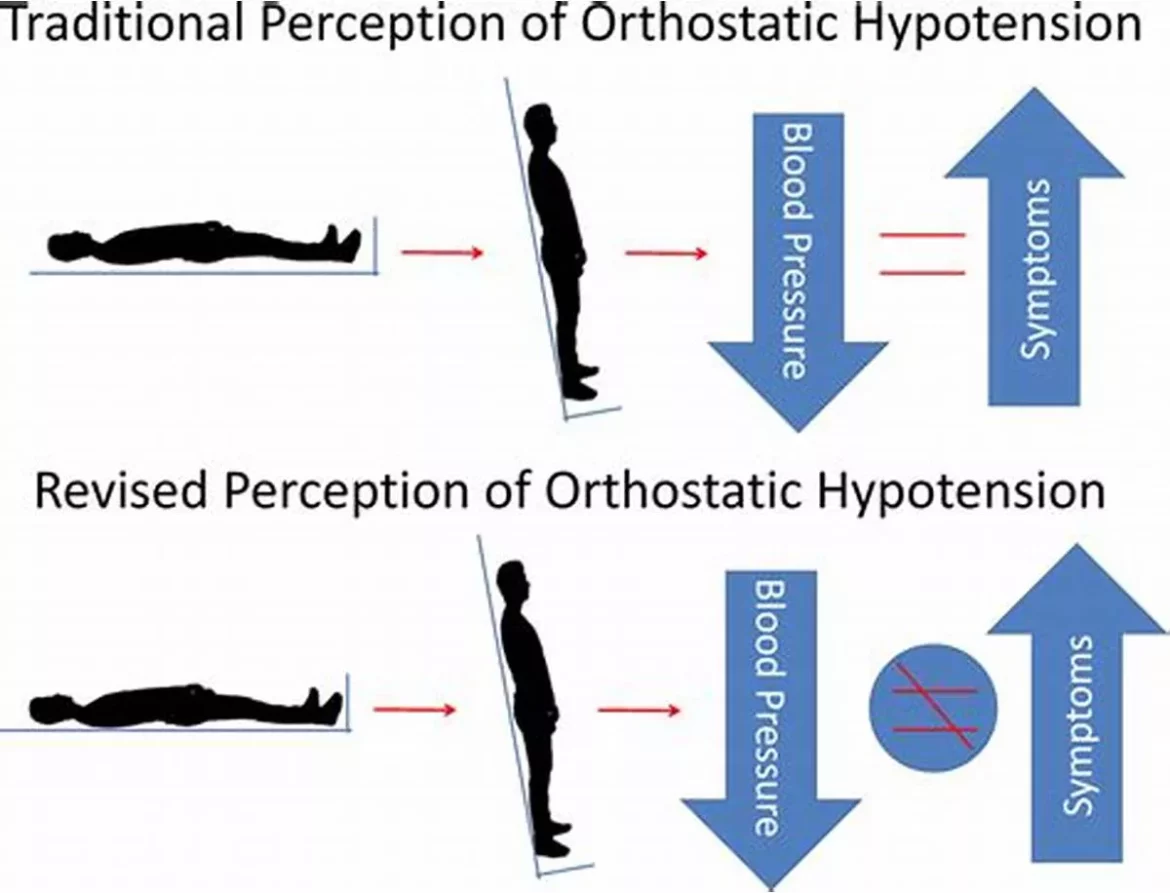
Orthostatic blood pressure, also known as orthostatic hypotension, is a condition characterized by a significant drop in blood pressure upon standing up from a sitting or lying position. This sudden decrease in blood pressure can lead to dizziness, lightheadedness, and even fainting. Understanding the causes of orthostatic blood pressure is crucial for effective management and prevention of associated complications. This article delves into the various factors contributing to orthostatic hypotension, providing a comprehensive overview of its underlying mechanisms and potential triggers.
Physiological Mechanisms
Blood Pressure Regulation
Blood pressure regulation is a complex process involving the heart, blood vessels, and autonomic nervous system. When a person stands up, gravity causes blood to pool in the lower extremities, reducing venous return to the heart. In response, baroreceptors in the carotid arteries and aorta sense the drop in blood pressure and trigger compensatory mechanisms.
These mechanisms include an increase in heart rate and vasoconstriction of blood vessels to maintain blood pressure and ensure adequate blood flow to the brain.
Autonomic Nervous System Dysfunction
One of the primary causes of orthostatic blood pressure is dysfunction of the autonomic nervous system, which regulates involuntary bodily functions, including blood pressure. Conditions such as autonomic neuropathy, often seen in diabetes, can impair the body’s ability to respond to postural changes, leading to inadequate compensatory mechanisms and subsequent hypotension.
Medical Conditions And Diseases
Neurological Disorders
Several neurological disorders can affect the autonomic nervous system and lead to orthostatic hypotension. Parkinson’s disease, multiple system atrophy, and pure autonomic failure are examples of conditions where autonomic dysfunction is prominent. These disorders can disrupt the neural pathways involved in blood pressure regulation, causing significant drops in blood pressure upon standing.
Cardiovascular Conditions
Cardiovascular conditions such as heart failure, myocardial infarction, and valvular heart disease can also contribute to orthostatic hypotension. These conditions can impair the heart’s ability to pump blood effectively, reducing cardiac output and making it difficult to maintain blood pressure when changing positions.
Endocrine Disorders
Endocrine disorders, including adrenal insufficiency (Addison’s disease) and hypothyroidism, can lead to orthostatic hypotension.
These conditions affect hormone levels that play a crucial role in maintaining blood pressure. For instance, cortisol deficiency in Addison’s disease can lead to reduced blood volume and vascular tone, resulting in orthostatic hypotension.
Medications
Antihypertensive Drugs
Medications used to treat high blood pressure, such as beta-blockers, diuretics, and alpha-blockers, can cause orthostatic hypotension as a side effect. These drugs lower blood pressure through various mechanisms, and their effects can be exacerbated by positional changes, leading to a significant drop in blood pressure upon standing.
Psychotropic Medications
Psychotropic medications, including antidepressants and antipsychotics, can also contribute to orthostatic hypotension.
These drugs can interfere with autonomic regulation and vascular tone, increasing the risk of hypotensive episodes when changing positions.
Other Medications
A wide range of other medications, such as nitrates used for angina, drugs for Parkinson’s disease, and certain sedatives, can cause orthostatic hypotension. The effects of these medications on blood pressure regulation should be closely monitored, especially in individuals at risk for hypotensive episodes.
Volume Depletion
Dehydration
Dehydration is a common cause of orthostatic hypotension. When the body is dehydrated, blood volume decreases, leading to reduced venous return to the heart and lower blood pressure. This condition is particularly common in older adults, who may have a diminished sense of thirst and be more susceptible to fluid loss.
Blood Loss
Acute or chronic blood loss can also lead to orthostatic hypotension.
Conditions such as gastrointestinal bleeding, heavy menstrual periods, or trauma can reduce blood volume, impairing the body’s ability to maintain stable blood pressure when changing positions.
Age-Related Changes
Reduced Baroreceptor Sensitivity
As people age, the sensitivity of baroreceptors decreases, making it more difficult for the body to detect and respond to changes in blood pressure. This reduced sensitivity can lead to inadequate compensatory mechanisms and a higher risk of orthostatic hypotension in older adults.
Decreased Cardiovascular Reserve
Older adults often have a reduced cardiovascular reserve, meaning their heart and blood vessels are less able to respond to stressors and maintain stable blood pressure. This decreased reserve can contribute to orthostatic hypotension, particularly in individuals with preexisting cardiovascular conditions.
Lifestyle Factors
Prolonged Bed Rest
Prolonged bed rest or immobility can lead to deconditioning of the cardiovascular system, making it more difficult for the body to regulate blood pressure upon standing. This can be a significant issue for hospitalized patients or those with chronic illnesses that limit mobility.
Physical Deconditioning
Lack of regular physical activity can also contribute to orthostatic hypotension. Physical deconditioning weakens the cardiovascular system, reducing its ability to respond effectively to postural changes and maintain stable blood pressure.
Diagnosis And Management
Diagnostic Evaluation
Diagnosing orthostatic hypotension involves a thorough clinical evaluation, including a detailed medical history, physical examination, and specific tests to measure blood pressure and heart rate changes upon standing. Additional tests, such as blood tests, ECG, and autonomic function tests, may be required to identify underlying causes and guide treatment.
Lifestyle Modifications
Lifestyle modifications can play a significant role in managing orthostatic hypotension. Increasing fluid and salt intake, wearing compression stockings, and avoiding sudden position changes can help mitigate symptoms. Regular physical activity and exercises to strengthen the cardiovascular system can also be beneficial.
Medical Treatment
Medical treatment for orthostatic hypotension may involve adjusting or discontinuing medications that contribute to the condition. In some cases, medications such as fludrocortisone or midodrine may be prescribed to help increase blood volume or vascular tone. Treating underlying medical conditions, such as diabetes or Parkinson’s disease, is also crucial for managing orthostatic hypotension.
Conclusion
Orthostatic blood pressure, or orthostatic hypotension, is a condition with multiple potential causes, ranging from autonomic nervous system dysfunction and cardiovascular conditions to medication side effects and lifestyle factors.
Understanding the underlying mechanisms and triggers is essential for effective diagnosis and management. By addressing the root causes and implementing appropriate lifestyle and medical interventions, individuals with orthostatic hypotension can reduce their symptoms and improve their quality of life.