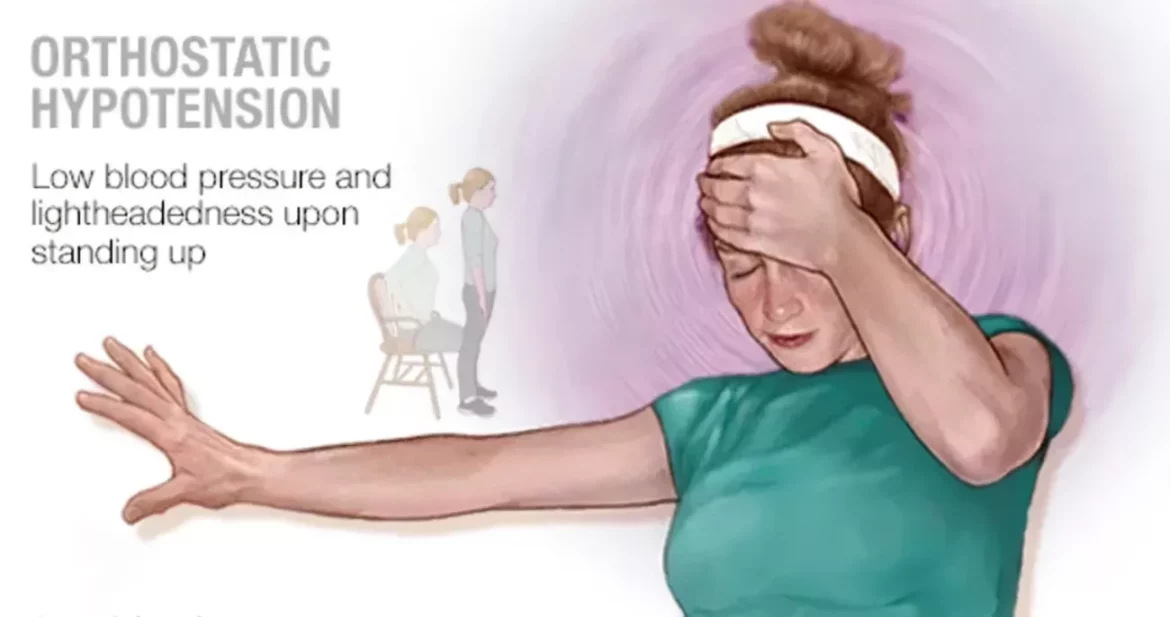
Postural hypotension, also known as orthostatic hypotension, is a form of low blood pressure that happens when you stand up from sitting or lying down. This condition can cause dizziness, lightheadedness, or even fainting. Understanding the underlying causes of postural hypotension is crucial for managing the condition and improving patient outcomes. This article will explore the various reasons for postural hypotension, the mechanisms behind it, and its potential impact on health.
What Is Blood Pressure Regulation?
Blood pressure is the force exerted by circulating blood on the walls of blood vessels. It is primarily regulated by the autonomic nervous system, which adjusts the diameter of blood vessels and the rate of the heart to maintain stable blood pressure levels. When a person stands up, gravity causes blood to pool in the lower extremities. To counteract this, the body must quickly adjust by narrowing the blood vessels and increasing the heart rate to maintain adequate blood flow to the brain. If these adjustments are insufficient or delayed, postural hypotension can occur.
See Also: what causes exercise induced hypertension
Primary Causes of Postural Hypotension
1. Dehydration
Dehydration is a common cause of postural hypotension. When the body lacks adequate fluids, blood volume decreases, making it difficult for the cardiovascular system to maintain stable blood pressure upon standing. Symptoms of dehydration include dry mouth, excessive thirst, reduced urine output, and fatigue.
2. Medications
Several types of medications can lead to postural hypotension by affecting blood pressure regulation. These include:
Diuretics: Used to treat high blood pressure and heart failure, diuretics increase urine output, potentially leading to dehydration and decreased blood volume.
Alpha-blockers: Prescribed for high blood pressure or prostate problems, these medications can cause blood vessels to remain too dilated, lowering blood pressure.
Beta-blockers: While effective in treating high blood pressure and heart conditions, beta-blockers can reduce the heart rate too much, impairing the body’s ability to adjust blood pressure upon standing.
Antidepressants: Certain antidepressants, particularly tricyclics, can interfere with the autonomic nervous system’s regulation of blood pressure.
See Also: what to do for orthostatic hypertension
3. Heart Problems
Various heart conditions can contribute to postural hypotension by impairing the heart’s ability to pump blood effectively.
These include:
Heart failure: Reduced heart function means less efficient blood circulation, making it harder to maintain blood pressure when changing positions.
Bradycardia: An abnormally slow heart rate can prevent adequate blood flow adjustments upon standing.
Heart valve issues: Problems with heart valves can affect blood flow dynamics, leading to postural hypotension.
4. Nervous System Disorders
Disorders affecting the autonomic nervous system can disrupt the body’s ability to regulate blood pressure. Such conditions include:
Parkinson’s disease: This neurodegenerative disorder can impair autonomic functions, including blood pressure regulation.
Multiple system atrophy: A progressive condition affecting multiple parts of the nervous system, leading to severe autonomic dysfunction.
Diabetic neuropathy: Long-term diabetes can damage autonomic nerves, affecting blood pressure control.
5. Blood Volume Changes
Sudden changes in blood volume can lead to postural hypotension.
These changes can occur due to:
Acute blood loss: Hemorrhage or severe injury can significantly reduce blood volume, leading to postural hypotension.
Anemia: A lower red blood cell count reduces the blood’s oxygen-carrying capacity, impairing the body’s ability to maintain blood pressure.
Fluid loss from vomiting or diarrhea: These conditions can quickly deplete body fluids, reducing blood volume.
6. Endocrine Problems
Hormonal imbalances can affect blood pressure regulation. Conditions that may cause postural hypotension include:
Adrenal insufficiency (Addison’s disease): Insufficient production of cortisol and aldosterone, hormones crucial for maintaining blood pressure, can lead to postural hypotension.
Diabetes: Poorly controlled diabetes can lead to autonomic neuropathy, affecting blood pressure regulation.
Mechanisms Behind Postural Hypotension
1. Impaired Baroreceptor Reflex
Baroreceptors are specialized nerve endings located in the walls of blood vessels, particularly in the carotid arteries and aorta. They detect changes in blood pressure and send signals to the brain to initiate corrective actions. In postural hypotension, the baroreceptor reflex may be impaired, leading to delayed or inadequate responses to changes in body position.
2. Vascular Dilation
Excessive dilation of blood vessels can result in a significant drop in blood pressure upon standing. This can occur due to medications, autonomic nervous system dysfunction, or other underlying health conditions. When blood vessels do not constrict adequately, the blood pools in the lower extremities, reducing the amount available to maintain cerebral perfusion.
3. Cardiac Output Reduction
The heart’s ability to pump blood effectively is crucial for maintaining blood pressure. Conditions that reduce cardiac output, such as heart failure or bradycardia, can impair the body’s ability to adjust to postural changes. A reduced stroke volume or heart rate can lead to inadequate blood flow to the brain upon standing, causing symptoms of postural hypotension.
4. Blood Volume Depletion
A decrease in circulating blood volume can significantly impact blood pressure regulation. Dehydration, blood loss, or conditions like anemia reduce the overall blood volume, making it difficult for the cardiovascular system to maintain adequate pressure when transitioning from a supine to an upright position.
Impact of Postural Hypotension on Health
1. Increased Fall Risk
Postural hypotension can lead to dizziness and fainting, significantly increasing the risk of falls and related injuries, particularly in older adults. Falls can result in fractures, head injuries, and a decline in overall mobility and independence.
2. Cognitive Impairment
Chronic postural hypotension can lead to reduced cerebral perfusion, potentially impacting cognitive function. Symptoms may include difficulty concentrating, memory problems, and general cognitive decline. In severe cases, this can contribute to conditions like dementia.
3. Cardiovascular Complications
Frequent episodes of postural hypotension can strain the cardiovascular system, potentially leading to more serious complications. These include an increased risk of stroke, heart attack, and other cardiovascular events due to the repeated stress of maintaining blood pressure.
4. Reduced Quality of Life
The symptoms of postural hypotension, such as dizziness, lightheadedness, and fatigue, can significantly impact daily activities and overall quality of life. Individuals may become fearful of standing or walking, leading to reduced physical activity and social engagement.
Managing Postural Hypotension
1. Lifestyle Modifications
Making certain lifestyle changes can help manage postural hypotension:
Hydration: Ensuring adequate fluid intake is crucial for maintaining blood volume and preventing dehydration.
Salt intake: Increasing salt intake, under medical supervision, can help raise blood pressure.
Small, frequent meals: Eating smaller, more frequent meals can prevent postprandial drops in blood pressure.
Gradual position changes: Slowly transitioning from lying down to sitting, and then to standing, can give the body more time to adjust.
2. Medications
Certain medications can help manage postural hypotension:
Fludrocortisone: This corticosteroid helps increase blood volume and improve blood pressure.
Midodrine: An alpha-adrenergic agonist that constricts blood vessels, raising blood pressure.
Pyridostigmine: Enhances neurotransmission in the autonomic nervous system, improving blood pressure regulation.
3. Physical Countermaneuvers
Specific physical maneuvers can help prevent a drop in blood pressure upon standing:
Leg crossing: Crossing the legs while standing can help increase blood pressure.
Squatting: Briefly squatting can aid in venous return and stabilize blood pressure.
Isometric exercises: Performing isometric exercises, such as handgrip exercises, can temporarily raise blood pressure.
4. Compression Garments
Wearing compression stockings or abdominal binders can help prevent blood pooling in the lower extremities and support blood pressure regulation.
5. Monitoring and Follow-Up
Regular monitoring of blood pressure and follow-up with a healthcare provider are essential for managing postural hypotension. Adjustments to treatment plans may be necessary based on the individual’s response and any underlying conditions.
Conclusion
Postural hypotension is a complex condition with multiple underlying causes. Understanding the reasons for postural hypotension is crucial for effective management and prevention of complications. By addressing factors such as dehydration, medication side effects, heart problems, nervous system disorders, and blood volume changes, individuals and healthcare providers can work together to mitigate the impact of this condition on daily life and overall health. With appropriate lifestyle modifications, medications, and monitoring, the symptoms of postural hypotension can be managed effectively, improving the quality of life for those affected.