Portal hypertensive gastropathy (PHG) is a condition that arises as a consequence of portal hypertension, which is an increase in blood pressure within the portal vein system. This condition is often seen in patients with liver cirrhosis and can lead to significant morbidity due to its impact on the stomach lining. Understanding the symptoms of PHG is crucial for early diagnosis and management, which can improve patient outcomes and quality of life.
Understanding Portal Hypertension And Its Impact
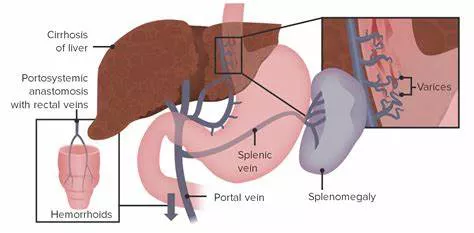
Portal hypertension occurs when there is increased resistance to blood flow through the liver, often due to liver cirrhosis, fibrosis, or other liver diseases. The increased pressure in the portal vein causes the formation of collateral blood vessels and affects various organs, including the stomach. When the stomach lining is exposed to high portal pressures, it can lead to changes in the mucosa, known as portal hypertensive gastropathy.
See Also:what are the symptoms of postural hypertension
What Are The Symptoms of Portal Hypertensive Gastropathy?
1. Gastrointestinal Bleeding
Gastrointestinal (GI) bleeding is one of the most significant symptoms of PHG. It can present in various forms, such as:
Hematemesis: Vomiting blood, which may be fresh (bright red) or altered (coffee-ground appearance) due to partial digestion by stomach acid.
Melena: Black, tarry stools indicating the presence of digested blood from the upper GI tract.
Occult Bleeding: Microscopic blood loss that may not be immediately visible but can lead to chronic anemia.
See Also: what are the symptoms of essential hypertension
2. Anemia
Due to chronic blood loss from the stomach, patients with PHG often develop anemia. Symptoms of anemia may include:
- Fatigue and weakness
- Pallor (pale skin and mucous membranes)
- Shortness of breath, especially on exertion
- Dizziness or lightheadedness
3. Epigastric Pain and Discomfort
Patients with PHG may experience epigastric pain or discomfort, which is located in the upper abdomen, just below the rib cage. This pain can vary in intensity and may be related to meal consumption.
4. Nausea and Vomiting
Nausea and vomiting are common symptoms in patients with PHG. These symptoms can be exacerbated by the presence of bleeding or significant mucosal damage in the stomach.
5. Early Satiety
Early satiety, or the feeling of fullness after consuming a small amount of food, can occur in PHG due to changes in the stomach lining and blood flow. This can lead to unintentional weight loss and malnutrition if not managed appropriately.
Pathophysiology of Portal Hypertensive Gastropathy
The pathophysiology of PHG involves complex hemodynamic changes due to portal hypertension. Increased pressure in the portal vein leads to:
Mucosal Congestion: The blood vessels in the stomach mucosa become dilated and congested, leading to the characteristic appearance of a “snake-skin” or mosaic pattern on endoscopy.
Increased Vascular Permeability: The congestion and dilation of blood vessels increase vascular permeability, making the mucosa more susceptible to bleeding.
Altered Mucosal Defense Mechanisms: Chronic liver disease can impair the stomach’s mucosal defenses, including reduced mucus production and decreased bicarbonate secretion, which can exacerbate mucosal injury.
Diagnosis of Portal Hypertensive Gastropathy
Diagnosis of PHG primarily relies on endoscopic examination. The characteristic findings include:
Mosaic Pattern: A snake-skin appearance of the gastric mucosa, which is indicative of PHG.
Erosions and Ulcers: In severe cases, the mucosa may develop erosions or ulcers, which can lead to bleeding.
Portal Hypertensive Collaterals: The presence of dilated blood vessels or varices in the stomach.
Management of Portal Hypertensive Gastropathy
The management of PHG focuses on controlling portal hypertension and preventing or treating bleeding. Strategies include:
1. Pharmacological Therapy
Non-selective Beta-Blockers: Medications such as propranolol and nadolol reduce portal pressure by decreasing cardiac output and splanchnic blood flow.
Vasoactive Drugs: Agents like octreotide and terlipressin can reduce portal pressure and control acute bleeding episodes.
2. Endoscopic Therapy
Endoscopic Variceal Ligation (EVL): Used for treating esophageal varices, which often coexist with PHG.
Endoscopic Sclerotherapy: Involves the injection of sclerosing agents into bleeding vessels to control hemorrhage.
3. Radiological Interventions
Transjugular Intrahepatic Portosystemic Shunt (TIPS): A procedure that creates a pathway between the portal vein and hepatic vein to reduce portal pressure. TIPS is effective in reducing the risk of bleeding from PHG.
4. Surgical Options
Liver Transplantation: In cases of severe liver disease and refractory portal hypertension, liver transplantation may be considered.
Prevention And Monitoring
Preventing complications of PHG involves regular monitoring and managing underlying liver disease. Key preventive measures include:
Regular Endoscopic Surveillance: Periodic endoscopy to monitor the severity of PHG and detect early signs of bleeding.
Liver Disease Management: Controlling the underlying liver disease through lifestyle modifications, medications, and, if necessary, antiviral therapy for viral hepatitis.
Nutritional Support: Ensuring adequate nutrition to prevent malnutrition and support liver function.
Conclusion
Portal hypertensive gastropathy is a significant complication of portal hypertension, primarily affecting patients with liver cirrhosis. Recognizing the symptoms, such as gastrointestinal bleeding, anemia, epigastric pain, nausea, vomiting, and early satiety, is crucial for timely diagnosis and management. Endoscopic evaluation remains the cornerstone of diagnosis, while management strategies focus on reducing portal pressure and preventing bleeding. Regular monitoring and comprehensive management of underlying liver disease are essential in improving patient outcomes and quality of life in those affected by PHG.