Portal hypertension is a significant medical condition that arises from increased blood pressure within the portal venous system, which includes the veins coming from the stomach, intestine, spleen, and pancreas that merge into the portal vein and subsequently branch into smaller vessels within the liver. Understanding the symptoms associated with portal hypertension is crucial for timely diagnosis and management. This article delves into the five main symptoms of portal hypertension, providing comprehensive insights into each.
What Are 5 The Main Symptoms of Portal Hypertension
1. Variceal Bleeding
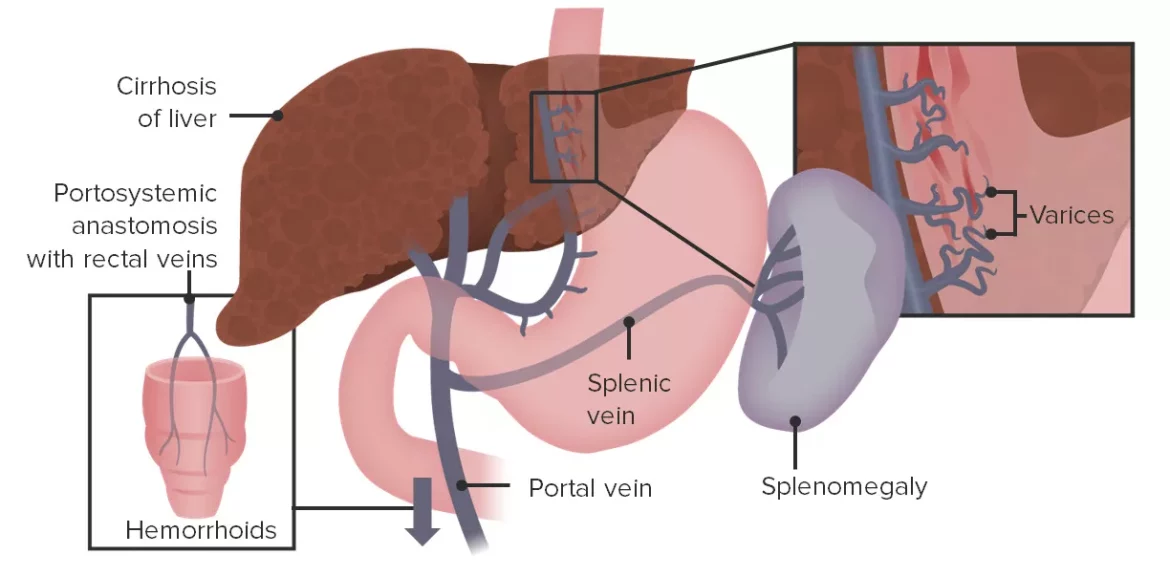
Variceal bleeding is one of the most severe and life-threatening complications of portal hypertension. It occurs when high pressure in the portal vein causes veins in the esophagus or stomach to enlarge and potentially rupture. This bleeding can lead to significant blood loss and requires immediate medical attention.
Causes and Mechanism
Varices develop due to the formation of collateral circulation as the body attempts to bypass the high-pressure portal system. These varices are thin-walled and prone to rupture under increased pressure. Esophageal varices are particularly vulnerable and can cause massive gastrointestinal bleeding.
Symptoms and Diagnosis
Patients with variceal bleeding may present with hematemesis (vomiting blood), melena (black, tarry stools), or hematochezia (passing fresh blood through the rectum). Diagnosis is typically confirmed through endoscopy, which allows direct visualization of the varices and the source of bleeding.
Management
Management of variceal bleeding involves stabilizing the patient, controlling the hemorrhage, and preventing recurrence.
Initial treatment may include endoscopic variceal ligation (banding), sclerotherapy, or the use of medications like vasopressin analogs to reduce portal pressure. In severe cases, a transjugular intrahepatic portosystemic shunt (TIPS) may be necessary.
See Also: What are the symptoms of portal hypertensive gastropathy?
2. Ascites
Ascites is the accumulation of fluid in the peritoneal cavity, often seen in advanced liver disease associated with portal hypertension. It is a common and debilitating symptom that significantly impacts the quality of life.
Pathophysiology
The development of ascites is multifactorial, involving increased hydrostatic pressure in the portal vein, reduced oncotic pressure due to hypoalbuminemia, and renal retention of sodium and water. These factors collectively lead to fluid leakage into the abdominal cavity.
Clinical Presentation
Patients with ascites may experience abdominal distension, discomfort, and difficulty breathing due to increased intra-abdominal pressure. Physical examination typically reveals a distended abdomen with a fluid wave or shifting dullness.
Diagnostic Approach
Diagnosis of ascites involves clinical evaluation and imaging studies such as ultrasound or CT scans to confirm fluid accumulation. Paracentesis, the removal of ascitic fluid, is performed to analyze the fluid for signs of infection (spontaneous bacterial peritonitis) and to assess its etiology.
Treatment Strategies
Management includes dietary sodium restriction, diuretics (e.g., spironolactone and furosemide), and large-volume paracentesis for symptomatic relief. Refractory ascites may require TIPS or liver transplantation.
See Also: what are symptoms of too low blood pressure
3. Hepatic Encephalopathy
Hepatic encephalopathy is a neuropsychiatric syndrome resulting from liver dysfunction and portosystemic shunting, leading to the accumulation of neurotoxins, particularly ammonia, which affects brain function.
Etiology and Pathogenesis
The impaired liver function in portal hypertension fails to detoxify substances from the gut, which then enter the systemic circulation and reach the brain. Ammonia, produced by intestinal bacteria and protein metabolism, plays a central role in the pathogenesis of hepatic encephalopathy.
Symptoms and Clinical Stages
Symptoms range from subtle cognitive changes and sleep disturbances to severe confusion, disorientation, and coma.
The West Haven Criteria classify hepatic encephalopathy into four stages, from mild (Grade I) to severe (Grade IV).
Diagnosis
Diagnosis is primarily clinical, supported by elevated blood ammonia levels and neuropsychological testing. Imaging studies such as MRI can help exclude other causes of altered mental status.
Management
Treatment focuses on reducing blood ammonia levels through dietary protein restriction, lactulose (a non-absorbable disaccharide that traps ammonia in the gut), and antibiotics like rifaximin to decrease intestinal ammonia production.
4. Splenomegaly and Hypersplenism
Splenomegaly, or an enlarged spleen, is another hallmark of portal hypertension, often leading to hypersplenism, a condition where the spleen excessively sequesters and destroys blood cells.
Mechanism and Impact
The increased pressure in the splenic vein, a part of the portal system, causes spleen enlargement. Hypersplenism results in thrombocytopenia (low platelet count), leukopenia (low white blood cell count), and anemia (low red blood cell count) due to increased destruction or sequestration of these cells.
Clinical Manifestations
Patients may present with a feeling of fullness or discomfort in the left upper abdomen due to splenic enlargement. They may also experience symptoms related to pancytopenia, such as easy bruising, frequent infections, and fatigue.
Diagnostic Evaluation
Splenomegaly is typically detected through physical examination and confirmed with imaging studies like ultrasound or CT scan. Blood tests reveal cytopenias indicative of hypersplenism.
Treatment Approaches
Management may include addressing the underlying portal hypertension, supportive care for cytopenias, and in some cases, splenectomy (surgical removal of the spleen) if hypersplenism is severe and symptomatic.
5. Hepatorenal Syndrome
Hepatorenal syndrome (HRS) is a serious complication of advanced liver disease characterized by renal failure due to altered renal blood flow, in the absence of any intrinsic kidney pathology.
Pathophysiology
The exact mechanism involves intense vasoconstriction of renal arteries and reduced renal perfusion due to systemic vasodilation caused by liver failure and portal hypertension. This leads to a functional decline in kidney function without any structural damage.
Clinical Features
Patients with HRS present with oliguria (low urine output), azotemia (elevated blood urea nitrogen and creatinine), and signs of fluid overload. HRS is classified into two types: Type 1 is a rapidly progressive renal failure, while Type 2 is a more chronic and less severe form.
Diagnostic Criteria
Diagnosis is based on clinical criteria, including severe liver disease with portal hypertension, low urine sodium concentration, and exclusion of other causes of renal failure. Diagnostic tests also include renal ultrasound to rule out obstructive causes.
Treatment Options
Management includes addressing the underlying liver disease and supportive care. Vasoconstrictors like terlipressin, combined with albumin infusions, are used to improve renal perfusion. Liver transplantation is the definitive treatment for HRS.
Conclusion
Portal hypertension manifests through various symptoms that reflect the underlying pathophysiological changes in the liver and its circulatory system. Recognizing these symptoms early can lead to prompt diagnosis and management, improving patient outcomes. Comprehensive understanding and timely intervention are crucial in managing the complications associated with portal hypertension, ultimately enhancing the quality of life for affected individuals.