Hyperlipidemia, characterized by elevated levels of lipids (fats) in the blood, can be influenced by various factors, including diet, lifestyle, genetics, and medications. Understanding the impact of medications on lipid levels is crucial for managing and mitigating the risk of cardiovascular diseases. This article delves into the specific medications that can cause hyperlipidemia, exploring their mechanisms, clinical implications, and management strategies.
Types of Hyperlipidemia
There are several types of hyperlipidemia, classified based on the specific lipid abnormalities:
Hypercholesterolemia: Elevated levels of total cholesterol or low-density lipoprotein (LDL) cholesterol.
Hypertriglyceridemia: Elevated levels of triglycerides.
Mixed Hyperlipidemia: Elevated levels of both cholesterol and triglycerides.
What Medications Can Cause Hyperlipidemia?
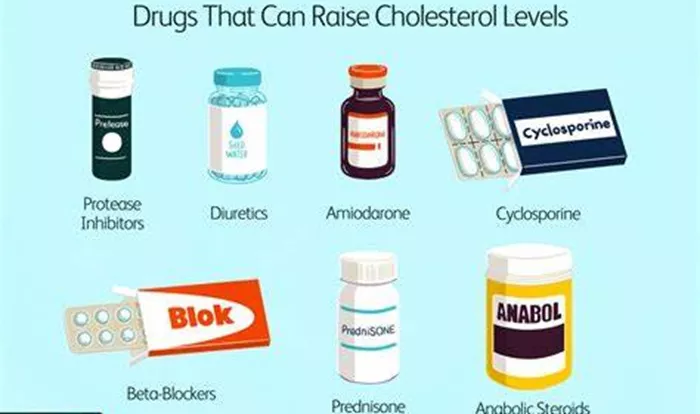
Several medications can contribute to hyperlipidemia by altering lipid metabolism, increasing lipid production, or reducing lipid clearance.
These medications can be categorized based on their primary use and mechanisms of action.
See Also: Mixed Hyperlipidemia Vs High Cholesterol : What Is The Same
1. Corticosteroids
Corticosteroids, such as prednisone and dexamethasone, are commonly prescribed for inflammatory and autoimmune conditions.
They can induce hyperlipidemia by:
Increasing the production of very-low-density lipoprotein (VLDL) in the liver.
Reducing the clearance of LDL cholesterol.
Increasing triglyceride levels by promoting lipolysis in adipose tissue.
see also: Why Does Hyperlipidemia Cause Hyponatremia
2. Antipsychotics
Antipsychotic medications, particularly atypical antipsychotics like olanzapine, clozapine, and quetiapine, are used to treat psychiatric disorders such as schizophrenia and bipolar disorder. These drugs can cause hyperlipidemia by:
Increasing appetite and weight gain, leading to higher lipid levels.
Directly affecting lipid metabolism through their impact on insulin sensitivity and adipocyte function.
3. Immunosuppressants
Immunosuppressant drugs, including cyclosporine and tacrolimus, are used to prevent organ transplant rejection and treat autoimmune diseases. These medications can contribute to hyperlipidemia by:
Impairing lipid clearance from the bloodstream.
Increasing hepatic lipid synthesis.
4. Beta-Blockers
Beta-blockers, such as atenolol and metoprolol, are prescribed for hypertension, angina, and arrhythmias. They can cause hyperlipidemia by:
Reducing the activity of lipoprotein lipase, an enzyme involved in lipid metabolism.
Decreasing insulin sensitivity, leading to higher triglyceride levels.
5. Thiazide Diuretics
Thiazide diuretics, like hydrochlorothiazide and chlorthalidone, are commonly used to treat hypertension. They can induce hyperlipidemia by:
Increasing insulin resistance, which affects lipid metabolism.
Reducing the clearance of LDL cholesterol.
6. Oral Contraceptives
Oral contraceptives containing estrogen and progestin can affect lipid levels. Estrogen typically raises HDL cholesterol (good cholesterol) but can also increase triglycerides. Progestin can counteract some of estrogen’s effects, leading to variable impacts on lipid levels. The net effect on lipid levels depends on the specific formulation and dosage.
7. Retinoids
Retinoids, such as isotretinoin, used to treat severe acne, can cause hyperlipidemia by:
Increasing hepatic production of VLDL.
Reducing the clearance of triglycerides from the blood.
8. Protease Inhibitors
Protease inhibitors, used in the treatment of HIV, such as ritonavir and lopinavir, can induce hyperlipidemia by:
Increasing hepatic lipid synthesis.
Reducing the activity of lipoprotein lipase.
Causing insulin resistance, which affects lipid metabolism.
9. Antiepileptic Drugs
Certain antiepileptic drugs, like valproic acid and carbamazepine, can lead to hyperlipidemia by:
Increasing the synthesis of lipids in the liver.
Altering lipid metabolism through their effects on enzyme activity.
10. Anabolic Steroids
Anabolic steroids, often abused for performance enhancement, can cause hyperlipidemia by:
- Increasing LDL cholesterol levels.
- Reducing HDL cholesterol levels.
- Promoting hepatic lipid synthesis.
Mechanisms of Drug-Induced Hyperlipidemia
The mechanisms through which these medications induce hyperlipidemia are complex and multifaceted. Key mechanisms include:
1. Increased Lipid Production
Many medications stimulate the liver to produce more lipids, particularly VLDL, which subsequently increases LDL cholesterol and triglycerides in the bloodstream.
2. Reduced Lipid Clearance
Some drugs impair the clearance of lipids from the bloodstream by affecting the activity of enzymes like lipoprotein lipase or by interfering with receptor-mediated uptake of lipoproteins.
3. Altered Hormonal Balance
Medications that affect hormonal balance, such as oral contraceptives and anabolic steroids, can significantly impact lipid metabolism, leading to changes in cholesterol and triglyceride levels.
4. Increased Insulin Resistance
Several drugs, including corticosteroids, antipsychotics, and thiazide diuretics, can increase insulin resistance, which in turn affects lipid metabolism and leads to elevated triglyceride levels.
5. Weight Gain
Weight gain, a common side effect of many medications, can independently contribute to hyperlipidemia by increasing the synthesis and storage of lipids in adipose tissue.
Clinical Implications And Management
The clinical implications of drug-induced hyperlipidemia are significant, given the increased risk of cardiovascular diseases associated with elevated lipid levels. Managing this condition involves a multifaceted approach:
1. Medication Review and Adjustment
Healthcare providers should regularly review medications for their potential impact on lipid levels. If hyperlipidemia is detected, alternative medications with less impact on lipids should be considered when possible.
2. Lifestyle Modifications
Patients should be encouraged to adopt lifestyle changes that can help manage lipid levels, including:
Diet: A heart-healthy diet low in saturated fats and cholesterol can help reduce lipid levels.
Exercise: Regular physical activity can improve lipid profiles by increasing HDL cholesterol and reducing triglycerides.
Weight Management: Achieving and maintaining a healthy weight can significantly impact lipid levels.
3. Lipid-Lowering Medications
In some cases, lipid-lowering medications, such as statins, fibrates, or omega-3 fatty acids, may be necessary to manage elevated lipid levels caused by other medications.
4. Monitoring and Follow-Up
Regular monitoring of lipid levels is essential for patients taking medications known to cause hyperlipidemia. Follow-up appointments should focus on assessing the effectiveness of lifestyle changes and medication adjustments.
5. Patient Education
Educating patients about the potential side effects of their medications and the importance of lifestyle modifications can empower them to take an active role in managing their lipid levels.
Conclusion
Hyperlipidemia is a complex condition influenced by various factors, including medications. Understanding the specific drugs that can cause hyperlipidemia, their mechanisms, and the clinical implications is crucial for effective management.
By adopting a comprehensive approach that includes medication review, lifestyle modifications, and regular monitoring, healthcare providers can help patients maintain healthy lipid levels and reduce the risk of cardiovascular diseases.