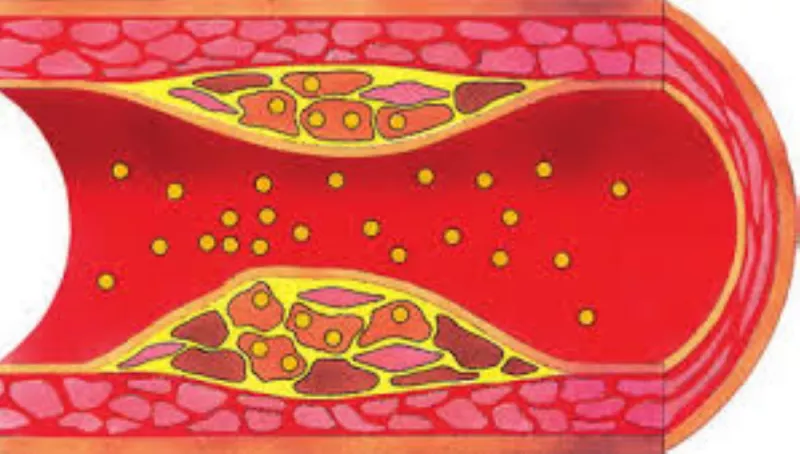
Hyperlipidemia, a condition characterized by elevated levels of lipids (fats) in the blood, including cholesterol and triglycerides, is a significant risk factor for cardiovascular diseases such as heart attack, stroke, and peripheral artery disease. Effective management of hyperlipidemia requires a multidisciplinary approach involving various healthcare professionals. This article will explore the roles of different specialists in treating hyperlipidemia, the strategies they employ, and the collaborative efforts necessary for optimal patient outcomes.
1. Primary Care Physicians (PCPs)
Primary care physicians, including family doctors and internists, are often the first point of contact for patients with hyperlipidemia. They play a crucial role in the initial diagnosis, management, and monitoring of the condition.
Diagnosis and Initial Assessment
Primary care physicians typically diagnose hyperlipidemia during routine check-ups or when patients present with risk factors such as obesity, hypertension, or a family history of cardiovascular disease. Diagnosis is confirmed through blood tests that measure total cholesterol, low-density lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL) cholesterol, and triglycerides.
Management and Treatment
Once diagnosed, PCPs initiate treatment based on the severity of the condition and the patient’s overall risk profile.
Management strategies include:
Lifestyle Modifications: PCPs educate patients on the importance of a heart-healthy diet, regular physical activity, weight management, and smoking cessation.
Medications: Depending on lipid levels and risk factors, PCPs may prescribe medications such as statins, fibrates, niacin, or omega-3 fatty acids.
Regular Monitoring: PCPs schedule regular follow-up appointments to monitor lipid levels and adjust treatment as necessary.
2. Cardiologists
Cardiologists are specialists in heart health and are often involved in the treatment of hyperlipidemia, particularly in patients with established cardiovascular disease or those at high risk.
Advanced Diagnostics and Risk Assessment
Cardiologists conduct comprehensive assessments to evaluate the risk of cardiovascular events. This may include advanced lipid testing, imaging studies such as coronary artery calcium scoring, and stress tests.
Intensive Treatment Protocols
For patients with high cardiovascular risk, cardiologists may recommend more intensive treatments, including:
High-Intensity Statin Therapy: Cardiologists often prescribe higher doses of statins or combination therapies to achieve lower LDL cholesterol targets.
PCSK9 Inhibitors: These newer injectable medications are used for patients who do not respond adequately to statins or have familial hypercholesterolemia.
Management of Comorbid Conditions: Cardiologists also manage other conditions that contribute to cardiovascular risk, such as hypertension and diabetes.
3. Endocrinologists
Endocrinologists specialize in hormone-related conditions and metabolic disorders, including diabetes and thyroid diseases, which are often associated with hyperlipidemia.
Treatment of Underlying Metabolic Disorders
Endocrinologists focus on identifying and treating underlying conditions that contribute to dyslipidemia:
Diabetes Management: Poorly controlled diabetes is a significant risk factor for hyperlipidemia. Endocrinologists optimize blood glucose control through medications, insulin therapy, and lifestyle interventions.
Thyroid Disorders: Hypothyroidism can lead to elevated cholesterol levels. Endocrinologists treat this condition with thyroid hormone replacement therapy.
Comprehensive Metabolic Control
Endocrinologists often employ a holistic approach to manage hyperlipidemia, addressing multiple metabolic factors simultaneously to achieve better lipid control and reduce cardiovascular risk.
4. Dietitians And Nutritionists
Dietitians and nutritionists are vital members of the healthcare team, providing specialized dietary counseling to help manage hyperlipidemia.
Personalized Dietary Plans
These professionals develop personalized nutrition plans based on the patient’s health status, preferences, and lifestyle. Key dietary recommendations may include:
Low Saturated Fat and Cholesterol Intake: Encouraging the consumption of lean meats, plant-based proteins, and low-fat dairy products.
Increased Fiber Intake: Promoting foods high in soluble fiber, such as oats, beans, fruits, and vegetables, which help lower cholesterol levels.
Healthy Fats: Recommending the inclusion of monounsaturated and polyunsaturated fats from sources like olive oil, nuts, and fatty fish.
Ongoing Support and Education
Dietitians and nutritionists provide ongoing support, monitoring dietary adherence, and making necessary adjustments to ensure long-term success in managing hyperlipidemia.
Pharmacists
Pharmacists play a crucial role in the management of hyperlipidemia, particularly in medication therapy management.
Medication Counseling
Pharmacists educate patients on the proper use of lipid-lowering medications, potential side effects, and the importance of adherence to prescribed treatments.
Medication Management
Pharmacists review patient medications to identify potential drug interactions, ensure appropriate dosing, and recommend alternatives if necessary.
Monitoring and Follow-Up
Pharmacists often work with other healthcare providers to monitor the effectiveness of therapy and make recommendations for adjustments based on patient response.
6. Nurse Practitioners (NPs) And Physician Assistants (PAs)
Nurse practitioners and physician assistants often work in collaboration with physicians to provide comprehensive care for patients with hyperlipidemia.
Patient Education and Lifestyle Counseling
NPs and PAs spend significant time educating patients about lifestyle changes, medication adherence, and the importance of regular monitoring.
Chronic Disease Management
These professionals are often involved in the long-term management of chronic conditions, providing regular follow-ups and coordinating care among different specialists.
7. Patient-Centered Care
The focus of interdisciplinary collaboration is on patient-centered care, involving the patient in decision-making and tailoring treatments to their preferences and lifestyle.
Conclusion
Treating hyperlipidemia is a multifaceted process that involves the expertise and collaboration of various healthcare professionals, including primary care physicians, cardiologists, endocrinologists, dietitians, pharmacists, nurse practitioners, and physician assistants. Each specialist brings a unique set of skills and knowledge to the table, contributing to a comprehensive and effective management plan. Through a combination of lifestyle modifications, medication therapy, and regular monitoring, patients with hyperlipidemia can achieve better lipid control, reduce their cardiovascular risk, and improve their overall health.