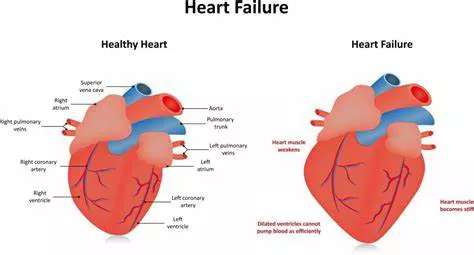
Heart failure, a condition where the heart cannot pump blood efficiently to meet the body’s needs, is a major health concern globally. It is broadly categorized into left heart failure and right heart failure, each presenting distinct signs and symptoms due to their differing pathophysiological mechanisms. Understanding these signs is crucial for early detection and effective management of heart failure. This article delves into the signs of left and right heart failure, exploring their causes, symptoms, and implications for patient care.
Signs of Left Heart Failure
1. Dyspnea (Shortness of Breath)
Dyspnea is one of the hallmark symptoms of left heart failure. It occurs because the left ventricle fails to effectively pump blood out to the body, causing a backlog of blood into the pulmonary veins. This congestion leads to fluid accumulation in the lungs, resulting in difficulty breathing. Patients often experience dyspnea during physical activities, and as the condition worsens, they may also experience it at rest.
2. Orthopnea and Paroxysmal Nocturnal Dyspnea
Orthopnea, or shortness of breath when lying flat, is a specific symptom of left heart failure. Patients may need to prop themselves up with pillows to breathe comfortably. Paroxysmal nocturnal dyspnea (PND) refers to sudden episodes of severe shortness of breath at night, waking the patient from sleep. Both conditions result from the redistribution of fluid from the lower extremities to the lungs when lying down, exacerbating pulmonary congestion.
See Also: Signs of A Weak Heart Valve
3. Fatigue and Weakness
Inadequate cardiac output in left heart failure leads to reduced oxygen and nutrient delivery to tissues, causing generalized fatigue and weakness. This symptom significantly impacts the patient’s quality of life, limiting their ability to perform daily activities.
4. Persistent Cough and Wheezing
The fluid buildup in the lungs can also cause a persistent cough, often producing frothy or blood-tinged sputum. Wheezing may occur due to bronchial congestion and airway obstruction. These respiratory symptoms are often mistaken for pulmonary conditions, highlighting the importance of accurate diagnosis.
5. Reduced Exercise Tolerance
Patients with left heart failure often report a diminished capacity for physical exertion. Activities that were once manageable become increasingly challenging, as the heart struggles to meet the elevated demands for blood flow during exercise. This reduced exercise tolerance is a key indicator of deteriorating cardiac function.
6. Nocturia
Nocturia, or frequent urination at night, is another symptom of left heart failure. It results from the improved renal perfusion and diuresis that occur when the patient is lying down, as well as the body’s attempt to excrete excess fluid accumulated during the day.
7. Pulmonary Edema
In severe cases, left heart failure can lead to acute pulmonary edema, a medical emergency characterized by extreme breathlessness, rapid breathing, a feeling of suffocation, and a sense of impending doom. The patient may also exhibit cyanosis (bluish discoloration of the skin) due to severe hypoxia. Immediate medical intervention is required to manage this life-threatening condition.
Signs of Right Heart Failure
1. Peripheral Edema
Peripheral edema, or swelling in the lower extremities, is a primary sign of right heart failure. It occurs because the right ventricle fails to pump blood efficiently to the lungs, causing blood to back up in the systemic veins. This venous congestion leads to fluid leakage into surrounding tissues, most commonly affecting the legs and ankles. The edema can progress to the abdomen (ascites) and even the scrotum in severe cases.
2. Jugular Venous Distension (JVD)
Jugular venous distension is another key sign of right heart failure. It is observed as a visible bulging of the jugular veins in the neck, reflecting increased central venous pressure due to the right heart’s inability to manage venous return. JVD is often assessed with the patient in a semi-recumbent position and is a reliable indicator of elevated right atrial pressure.
3. Hepatomegaly and Hepatojugular Reflux
Right heart failure can lead to hepatomegaly, or an enlarged liver, due to venous congestion in the hepatic veins. This condition may be accompanied by right upper quadrant abdominal pain. Hepatojugular reflux, a physical exam finding where gentle pressure applied over the liver results in increased jugular venous distension, is indicative of right heart failure and elevated right atrial pressure.
4. Ascites
Ascites, the accumulation of fluid in the peritoneal cavity, is a common sign of advanced right heart failure. It results from prolonged venous congestion and increased pressure in the hepatic and splanchnic circulation. Patients with ascites may experience abdominal discomfort, bloating, and a feeling of fullness.
5. Anorexia and Nausea
The gastrointestinal symptoms of anorexia and nausea are often seen in right heart failure due to congestion of the gastrointestinal tract. This congestion can impair digestion and absorption of nutrients, leading to weight loss and malnutrition in chronic cases.
6. Weight Gain
Despite the presence of anorexia, patients with right heart failure may experience unexplained weight gain due to fluid retention. Monitoring weight changes is crucial in managing heart failure, as sudden weight gain often indicates worsening fluid overload.
7. Fatigue and Weakness
Similar to left heart failure, fatigue and weakness are common symptoms of right heart failure. They are primarily due to reduced cardiac output and impaired blood flow to skeletal muscles, contributing to exercise intolerance and a decline in physical endurance.
Distinguishing Between Left And Right Heart Failure
While the signs of left and right heart failure are distinct, many patients with heart failure exhibit symptoms of both, a condition known as biventricular or congestive heart failure. It is essential to differentiate between the two to tailor treatment strategies effectively.
Clinical Examination And Diagnostic Tests
A thorough clinical examination, including a detailed patient history and physical assessment, is the first step in diagnosing heart failure. Diagnostic tests such as chest X-rays, echocardiograms, electrocardiograms (ECGs), and blood tests (e.g., B-type natriuretic peptide or BNP levels) provide valuable information on cardiac structure, function, and the extent of heart failure.
Management And Treatment
Management of heart failure involves a combination of lifestyle modifications, pharmacological therapy, and in some cases, surgical interventions. Treatment aims to alleviate symptoms, improve quality of life, and reduce the risk of hospitalization and mortality.
1. Lifestyle Modifications
Patients are advised to adhere to a heart-healthy diet, restrict sodium intake, engage in regular physical activity tailored to their condition, avoid excessive alcohol consumption, and quit smoking. Monitoring daily weight and fluid intake can help manage fluid retention and prevent exacerbations.
2. Pharmacological Therapy
Medications play a crucial role in managing heart failure. Commonly prescribed drugs include:
Diuretics: To reduce fluid overload and relieve symptoms of congestion.
ACE Inhibitors or ARBs: To lower blood pressure and reduce the heart’s workload.
Beta-blockers: To improve heart function and reduce mortality risk.
Aldosterone antagonists: To counteract the effects of aldosterone and prevent fluid retention.
Digoxin: In selected cases, to improve symptoms and exercise tolerance.
3. Surgical Interventions
In advanced cases of heart failure, surgical interventions such as coronary artery bypass grafting (CABG), valve repair or replacement, and implantation of devices like implantable cardioverter-defibrillators (ICDs) or cardiac resynchronization therapy (CRT) may be necessary. Heart transplantation is considered for patients with end-stage heart failure who do not respond to other treatments.
Conclusion
Recognizing the signs of left and right heart failure is vital for early diagnosis and effective management of this complex condition. While left heart failure primarily presents with respiratory symptoms due to pulmonary congestion, right heart failure is characterized by systemic venous congestion and its related symptoms. Comprehensive clinical assessment and appropriate diagnostic tests are essential for differentiating between the two and guiding treatment strategies. By understanding the signs and adopting a multidisciplinary approach to management, healthcare providers can significantly improve outcomes and quality of life for patients with heart failure.