Ventricular tachycardia (VT) is a type of fast heart rhythm that originates from the ventricles, the lower chambers of the heart. This condition is characterized by a heart rate that exceeds 100 beats per minute and can be life-threatening if not treated promptly. One of the hallmark features of VT on an electrocardiogram (ECG) is the widening of the QRS complex.
Understanding why the QRS complex is wide in VT requires a detailed look into the cardiac conduction system, the pathophysiology of ventricular tachycardia, and how these factors affect the morphology of the QRS complex.
The Cardiac Conduction System
The heart’s electrical conduction system is responsible for initiating and propagating electrical impulses that coordinate the contraction of the heart muscle. This system includes the sinoatrial (SA) node, atrioventricular (AV) node, bundle of His, bundle branches, and Purkinje fibers. Under normal circumstances, electrical impulses originate in the SA node, travel through the atria, and reach the AV node. From the AV node, the impulses travel through the bundle of His and then divide into the right and left bundle branches, which conduct the impulses to the ventricles, causing them to contract and pump blood.
See Also:What Is Arrhythmia Mean
What Is The QRS Complex?
The QRS complex is a crucial part of the ECG, representing the depolarization of the ventricles. This process involves the rapid spread of electrical impulses through the ventricles, leading to their contraction. In a normal ECG, the QRS complex is narrow, typically less than 120 milliseconds (ms) in duration. A narrow QRS complex indicates that the electrical impulses are traveling quickly and efficiently through the His-Purkinje system and the ventricular myocardium.
Pathophysiology of Ventricular Tachycardia
Ventricular tachycardia originates from the ventricles and is caused by abnormal electrical circuits within the ventricular myocardium. These circuits can be due to a variety of factors, including structural heart disease, ischemic heart disease, cardiomyopathy, and electrolyte imbalances. VT can be classified into monomorphic VT, where the QRS complexes have a uniform appearance, and polymorphic VT, where the QRS complexes vary in shape and size.
Why Is The QRS Complex Wide in Ventricular Tachycardia?
1. Abnormal Conduction Pathways
In ventricular tachycardia, the electrical impulses originate within the ventricles rather than the normal conduction pathways (SA node, AV node, and His-Purkinje system). When the impulses arise from an ectopic focus within the ventricles, they must travel through the ventricular myocardium rather than the specialized conduction fibers.
The myocardial tissue conducts impulses more slowly compared to the His-Purkinje system, leading to a delay in the spread of depolarization. This delay results in a prolonged QRS duration, making the QRS complex appear wide on the ECG.
2. Reentry Circuits
Reentry is a common mechanism underlying ventricular tachycardia. In this scenario, an electrical impulse repeatedly travels through a circular pathway within the ventricles, re-exciting the tissue as it goes. This reentrant circuit causes the ventricles to depolarize in an abnormal and prolonged manner, contributing to the widening of the QRS complex.
Reentry circuits often develop in areas of scar tissue or fibrosis, where the normal conduction pathways are disrupted.
3. Bundle Branch Block
In some cases of VT, one or both of the bundle branches may be involved in the abnormal conduction. This can result in a bundle branch block pattern on the ECG. When a bundle branch is blocked, the electrical impulses must travel through the myocardium rather than the rapid conduction fibers of the bundle branches. This leads to a delay in ventricular depolarization and results in a wide QRS complex.
4. Triggered Activity
Triggered activity is another mechanism that can cause VT and wide QRS complexes. This occurs when abnormal depolarizations are initiated by afterdepolarizations—abnormal electrical activity that follows the initial action potential. If these afterdepolarizations reach a threshold, they can trigger premature ventricular contractions and potentially lead to VT.
The abnormal site of origin and propagation of these impulses result in a wide QRS complex.
see also: Does Smoking Cause Arrhythmia
Clinical Significance of A Wide QRS Complex in VT
The presence of a wide QRS complex in VT is not just a diagnostic marker but also has clinical implications. A wide QRS complex indicates that the VT is originating from within the ventricles and is associated with a higher risk of hemodynamic instability. Patients with VT and a wide QRS complex are more likely to experience symptoms such as palpitations, dizziness, syncope, and in severe cases, cardiac arrest. The wide QRS complex helps clinicians differentiate VT from supraventricular tachycardia (SVT) with aberrant conduction, which is crucial for determining the appropriate treatment strategy.
Differentiating VT From SVT with Aberrant Conduction
One of the diagnostic challenges in cardiology is distinguishing VT from SVT with aberrant conduction, as both can present with wide QRS complexes. However, there are several ECG criteria and clinical features that can help differentiate these two conditions:
1. Capture and Fusion Beats
In VT, capture and fusion beats may be observed. A capture beat occurs when a normal sinus beat briefly “captures” the ventricles, resulting in a narrow QRS complex amidst the wide complexes of VT. A fusion beat is a hybrid of a normal sinus beat and a ventricular beat, resulting in a QRS complex with an intermediate width. These beats are not typically seen in SVT with aberrant conduction.
2. AV Dissociation
AV dissociation, where the atria and ventricles beat independently, is a hallmark of VT. In this situation, the P waves (representing atrial depolarization) and the QRS complexes are not related. This finding supports the diagnosis of VT rather than SVT with aberrant conduction.
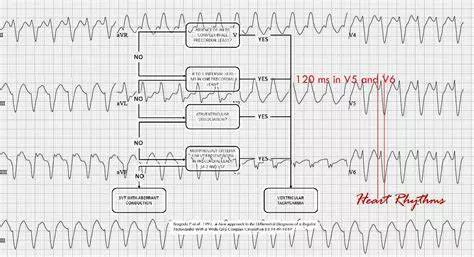
3. Brugada Criteria and Other ECG Algorithms
Several ECG algorithms, such as the Brugada criteria, can help differentiate VT from SVT with aberrant conduction. These criteria analyze the morphology of the QRS complexes and other ECG features to aid in diagnosis. For example, the presence of a monophasic R wave or an RS complex with a prolonged interval from onset to nadir (greater than 100 ms) in the precordial leads suggests VT.
Management of Ventricular Tachycardia
The management of VT depends on the patient’s hemodynamic stability and underlying cause of the arrhythmia. Acute management aims to restore normal heart rhythm and stabilize the patient, while long-term management focuses on preventing recurrences.
Acute Management
For hemodynamically stable patients with VT, antiarrhythmic medications such as amiodarone, procainamide, or lidocaine may be used to terminate the arrhythmia. For unstable patients, immediate synchronized cardioversion is indicated. In cases of cardiac arrest due to VT, defibrillation and advanced cardiac life support measures are required.
Long-Term Management
Long-term management strategies include:
1. Medications
Beta-blockers and antiarrhythmic drugs can help prevent recurrences of VT. Patients with structural heart disease or cardiomyopathy may benefit from medications that address the underlying condition.
2. Implantable Cardioverter-Defibrillator (ICD)
For patients at high risk of recurrent VT or sudden cardiac death, an ICD is recommended. This device continuously monitors the heart’s rhythm and delivers a shock if a life-threatening arrhythmia is detected.
3. Catheter Ablation
Catheter ablation is a procedure that targets and destroys the abnormal electrical pathways causing VT. This can be particularly effective in cases where the VT is due to a reentrant circuit.
4. Lifestyle Modifications and Risk Factor Management
Addressing risk factors such as hypertension, coronary artery disease, and electrolyte imbalances can help reduce the risk of VT. Lifestyle modifications, including maintaining a healthy weight, regular exercise, and avoiding stimulants, are also beneficial.
Conclusion
Understanding why the QRS complex is wide in ventricular tachycardia involves a comprehensive knowledge of the cardiac conduction system and the pathophysiology of VT. The abnormal origin and propagation of electrical impulses within the ventricles lead to a delay in depolarization, resulting in a wide QRS complex. This finding has significant diagnostic and clinical implications, helping differentiate VT from other tachyarrhythmias and guiding appropriate management strategies to improve patient outcomes.