Left ventricular diastolic dysfunction (LVDD) is a condition characterized by the heart’s inability to relax and fill properly during the diastolic phase, the part of the cardiac cycle when the heart relaxes after contraction. The left ventricle, which is responsible for pumping oxygenated blood to the body, requires a delicate balance between contraction (systole) and relaxation (diastole). When this balance is disrupted, it can lead to impaired filling and subsequent issues with blood circulation.
LVDD is often detected through echocardiography, which can reveal abnormal patterns of blood flow and ventricular relaxation. This condition can be classified into various grades, ranging from mild (Grade I) to severe (Grade III and IV), based on the severity of the dysfunction and the presence of additional symptoms such as increased left atrial pressure.
Diastolic Dysfunction Vs. Systolic Dysfunction
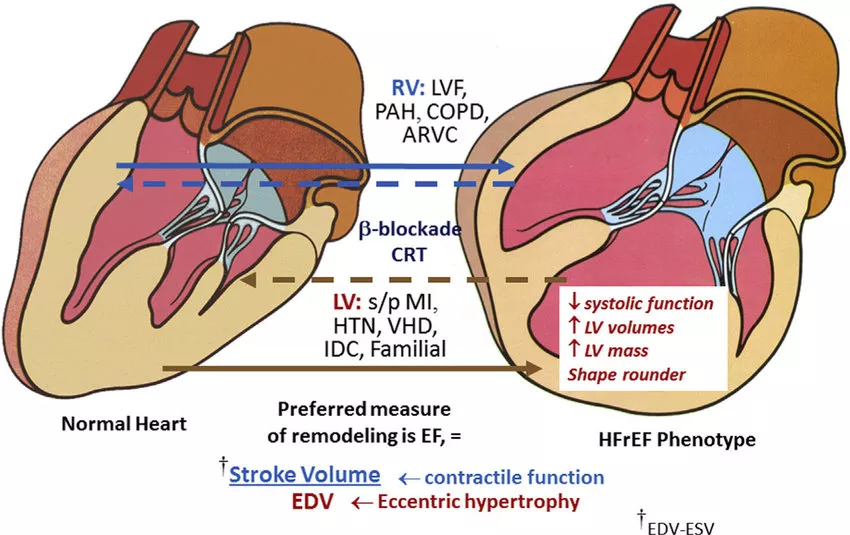
To fully grasp whether LVDD constitutes heart failure, it’s essential to differentiate between diastolic and systolic dysfunction. Systolic dysfunction involves the heart’s impaired ability to contract and pump blood effectively, often measured by a reduced ejection fraction (EF). Diastolic dysfunction, on the other hand, pertains to the heart’s impaired ability to relax and fill, which may not always affect the EF directly.
Heart failure can be broadly classified into two main types based on these dysfunctions:
Heart Failure with Reduced Ejection Fraction (HFrEF): This is commonly associated with systolic dysfunction, where the heart’s pumping ability is compromised.
Heart Failure with Preserved Ejection Fraction (HFpEF): This is often associated with diastolic dysfunction, where the heart’s relaxation and filling abilities are impaired despite a normal EF.
See Also: How Does Myocardial Infarction Cause Arrhythmia
Symptoms of Left Ventricular Diastolic Dysfunction
LVDD can present with various symptoms, many of which overlap with those of heart failure. These symptoms include:
Shortness of Breath: This can occur during exertion or at rest due to fluid buildup in the lungs (pulmonary congestion).
Fatigue and Weakness: Reduced cardiac output can lead to inadequate blood supply to the muscles, causing fatigue.
Swelling (Edema): Fluid retention can cause swelling in the lower extremities, abdomen, and other parts of the body.
Increased Heart Rate: The heart may beat faster to compensate for its impaired filling and pumping efficiency.
Difficulty Lying Flat: Patients may experience orthopnea, a condition where breathing becomes difficult when lying flat, often requiring the use of multiple pillows or sleeping in an upright position.
Diagnosis of Left Ventricular Diastolic Dysfunction
The diagnosis of LVDD typically involves a combination of clinical evaluation, imaging studies, and sometimes invasive procedures. Key diagnostic tools include:
Echocardiography: This is the primary tool for diagnosing LVDD. It provides detailed images of the heart’s structure and function, including measurements of ventricular filling pressures and relaxation patterns.
Electrocardiogram (ECG): This test records the electrical activity of the heart and can help identify abnormal rhythms or signs of left ventricular hypertrophy.
Blood Tests: Levels of natriuretic peptides (e.g., BNP or NT-proBNP) can be elevated in heart failure and may be used to assess the severity of the condition.
Cardiac Catheterization: In some cases, invasive measurements of pressures within the heart chambers may be necessary to confirm the diagnosis and assess the severity of diastolic dysfunction.
Causes And Risk Factors of Left Ventricular Diastolic Dysfunction
Several factors can contribute to the development of LVDD, including:
Aging: The natural aging process can lead to changes in the heart’s structure and function, including increased stiffness of the ventricular walls.
Hypertension: Chronic high blood pressure can cause the left ventricle to become thickened (hypertrophied) and less compliant, impairing its ability to relax.
Coronary Artery Disease: Reduced blood flow to the heart muscle can lead to ischemia and subsequent diastolic dysfunction.
Diabetes: This condition can affect the heart muscle directly, leading to changes in its structure and function.
Obesity: Excess body weight can increase the workload on the heart and contribute to diastolic dysfunction.
Atrial Fibrillation: This common arrhythmia can exacerbate diastolic dysfunction by impairing the atrial contribution to ventricular filling.
Heart Valve Disease: Conditions such as aortic stenosis or mitral regurgitation can affect the pressure and volume dynamics within the heart, leading to diastolic dysfunction.
see also:What Are The Signs of Left Ventricular Failure
Is Left Ventricular Diastolic Dysfunction Considered Heart Failure?
Diastolic Heart Failure (Heart Failure with Preserved Ejection Fraction)
LVDD is often associated with heart failure with preserved ejection fraction (HFpEF). In HFpEF, the heart’s ejection fraction remains within the normal range (typically 50% or higher), but the ventricles are stiff and unable to relax properly. This leads to elevated pressures in the left atrium and pulmonary circulation, resulting in symptoms of heart failure.
Management And Treatment of Left Ventricular Diastolic Dysfunction
Lifestyle Modifications
Exercise: Regular physical activity can improve cardiovascular fitness and help manage risk factors such as hypertension and obesity.
Diet: A heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins can support overall cardiovascular health.
Weight Management: Maintaining a healthy weight can reduce the burden on the heart and improve symptoms.
Medications
Antihypertensive Agents: Medications such as ACE inhibitors, angiotensin II receptor blockers (ARBs), and calcium channel blockers can help control blood pressure and reduce ventricular stiffness.
Diuretics: These medications can help manage fluid retention and reduce symptoms of congestion.
Beta-Blockers: These drugs can slow the heart rate, allowing more time for ventricular filling and improving diastolic function.
Aldosterone Antagonists: Medications like spironolactone can reduce fibrosis and improve ventricular compliance.
Management of Comorbidities
Diabetes Control: Effective management of blood glucose levels can reduce the risk of cardiovascular complications.
Management of Atrial Fibrillation: Rhythm control or rate control strategies, along with anticoagulation therapy, can reduce the impact of atrial fibrillation on diastolic function.
Advanced Therapies
In cases of severe HFpEF, more advanced therapies may be considered, including:
Cardiac Resynchronization Therapy (CRT): This therapy can improve coordination of ventricular contractions in select patients with electrical dyssynchrony.
Heart Transplantation: In end-stage heart failure, transplantation may be an option for eligible patients.
Prognosis And Long-Term Outlook
The prognosis for individuals with LVDD varies widely based on the severity of the dysfunction, the presence of symptoms, and associated comorbidities. Patients with asymptomatic LVDD may have a relatively benign course, while those with symptomatic HFpEF may experience a more challenging clinical trajectory.
It’s important to note that HFpEF carries a significant burden in terms of morbidity and mortality, comparable to that of heart failure with reduced ejection fraction (HFrEF). Therefore, early identification and management of LVDD and its underlying causes are crucial in improving outcomes and quality of life for affected individuals.
Conclusion
Left ventricular diastolic dysfunction represents a spectrum of conditions characterized by impaired relaxation and filling of the left ventricle. While LVDD itself may not always be synonymous with heart failure, it is a key component of heart failure with preserved ejection fraction (HFpEF). The distinction lies in the presence of symptoms and the impact on cardiac function.
Effective management of LVDD involves addressing underlying causes, optimizing medical therapy, and implementing lifestyle modifications.
By doing so, it is possible to mitigate symptoms, improve functional capacity, and enhance the overall prognosis for individuals with this condition. As our understanding of LVDD and HFpEF continues to evolve, ongoing research and advances in treatment strategies will play a crucial role in improving outcomes for patients with these complex and interrelated conditions.