Acute pancreatitis is a sudden inflammation of the pancreas that can lead to severe health complications, including hypotension.
Understanding the link between acute pancreatitis and hypotension is crucial for medical professionals and patients alike.
This article explores the underlying mechanisms, clinical implications, and management strategies associated with hypotension in the context of acute pancreatitis.
What Is Acute Pancreatitis?
Acute pancreatitis is characterized by the rapid onset of inflammation in the pancreas, an essential organ responsible for producing digestive enzymes and hormones such as insulin. This condition can range from mild discomfort to severe, life-threatening illness. The inflammation typically results from the premature activation of digestive enzymes within the pancreas, leading to autodigestion and tissue damage.
Causes And Risk Factors
Several factors can trigger acute pancreatitis, including:
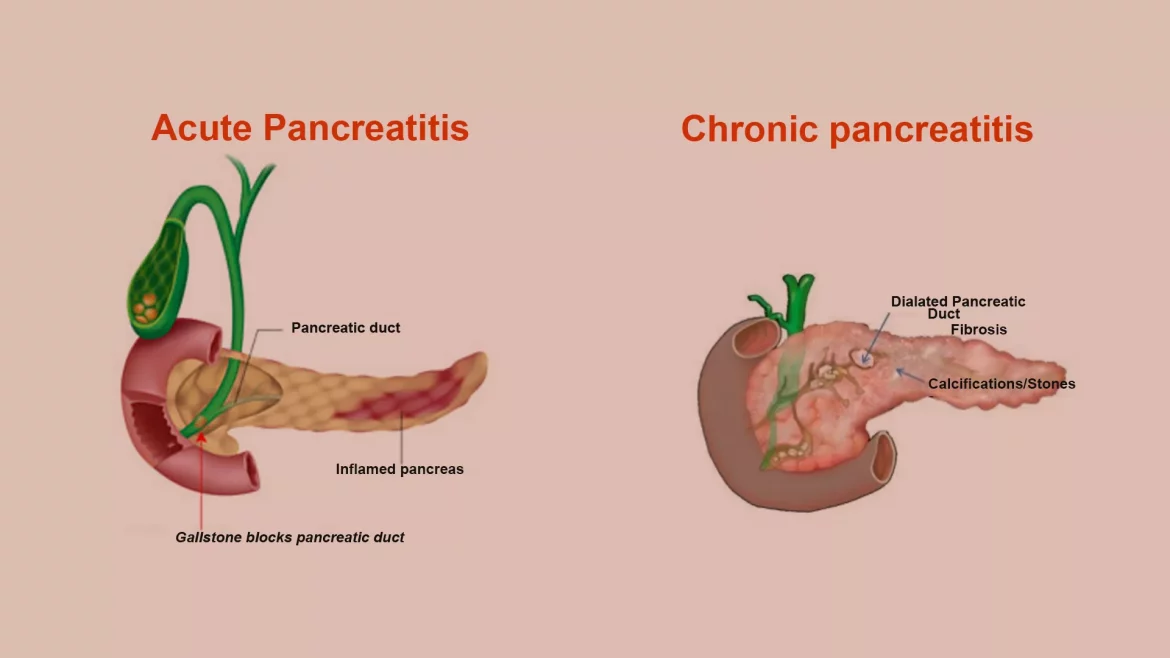
Gallstones: The most common cause, gallstones can block the pancreatic duct, leading to enzyme buildup and inflammation.
Chronic Alcohol Consumption: Excessive alcohol intake is a significant risk factor, contributing to approximately 30% of cases.
Medications: Certain drugs, such as corticosteroids and azathioprine, have been linked to acute pancreatitis.
Hypertriglyceridemia: Elevated triglyceride levels can precipitate the condition.
Infections: Viral infections like mumps or hepatitis can cause inflammation of the pancreas.
Trauma: Abdominal injury or surgical procedures can damage the pancreas, leading to acute pancreatitis.
see also: Why Does Sepsis Cause Hypotension?
Clinical Presentation
Patients with acute pancreatitis typically present with sudden onset of severe abdominal pain, often radiating to the back.
Other symptoms may include nausea, vomiting, fever, and a rapid pulse. Laboratory tests usually reveal elevated levels of pancreatic enzymes, such as amylase and lipase.
Why Does Acute Pancreatitis Cause Hypotension?
The relationship between acute pancreatitis and hypotension is complex and multifactorial. Several mechanisms contribute to the development of hypotension in this condition:
Systemic Inflammatory Response Syndrome (SIRS)
Acute pancreatitis often triggers a systemic inflammatory response. The release of inflammatory cytokines and mediators, such as tumor necrosis factor-alpha (TNF-α) and interleukins, can cause widespread vasodilation and increased vascular permeability. This leads to a significant drop in blood pressure.
Hypovolemia
In acute pancreatitis, fluid shifts from the intravascular space to the interstitial and retroperitoneal spaces due to increased capillary permeability. This fluid loss can result in hypovolemia, a critical factor in the development of hypotension.
Additionally, vomiting and reduced oral intake can exacerbate fluid deficits.
Cardiac Dysfunction
Severe cases of acute pancreatitis can lead to myocardial depression and cardiac dysfunction. The release of inflammatory mediators can impair myocardial contractility, reducing cardiac output and contributing to hypotension.
Sepsis and Infection
Acute pancreatitis can be complicated by infections, including pancreatic necrosis and abscess formation. The presence of infection can further exacerbate hypotension through septic shock, characterized by profound vasodilation and impaired perfusion.
see also: Will Water Reduce Blood Pressure?
Electrolyte Imbalances
Electrolyte disturbances, such as hypocalcemia and hyperkalemia, are common in acute pancreatitis. These imbalances can adversely affect cardiac function and vascular tone, leading to hypotension.
Clinical Implications And Management
Recognizing Hypotension in Acute Pancreatitis
Early recognition of hypotension in patients with acute pancreatitis is crucial for preventing complications and improving outcomes. Clinical signs of hypotension include:
Low Blood Pressure: Systolic blood pressure less than 90 mmHg.
Tachycardia: Rapid heart rate as a compensatory mechanism.
Cold, Clammy Skin: Indicative of poor perfusion.
Altered Mental Status: Confusion or decreased level of consciousness.
Diagnostic Approaches
Several diagnostic tools can aid in assessing hypotension in acute pancreatitis:
Hemodynamic Monitoring: Continuous monitoring of blood pressure, heart rate, and central venous pressure.
Laboratory Tests: Assessing electrolyte levels, renal function, and markers of inflammation and infection.
Imaging Studies: Ultrasound, CT scan, or MRI to evaluate pancreatic inflammation, necrosis, and fluid collections.
Treatment Strategies
The management of hypotension in acute pancreatitis involves addressing the underlying causes and supporting cardiovascular function. Key strategies include:
Fluid Resuscitation
Aggressive fluid replacement is the cornerstone of managing hypotension in acute pancreatitis. Isotonic crystalloids, such as normal saline or lactated Ringer’s solution, are typically administered to restore intravascular volume and improve perfusion. Fluid therapy should be guided by hemodynamic parameters and urine output.
Vasoactive Agents
In cases of refractory hypotension, vasoactive agents may be required to maintain adequate blood pressure. Medications such as norepinephrine or dopamine can be used to support vascular tone and cardiac output.
Electrolyte Management
Correcting electrolyte imbalances is essential for stabilizing cardiovascular function. Intravenous calcium gluconate may be administered to address hypocalcemia, while potassium levels should be carefully monitored and corrected as needed.
Nutritional Support
Adequate nutritional support is vital for recovery in acute pancreatitis. Enteral feeding is preferred over parenteral nutrition, as it helps maintain gut integrity and reduce the risk of infection.
Pain Management
Effective pain control is crucial for patient comfort and may also help reduce sympathetic stimulation, which can contribute to hypotension. Opioids and other analgesics should be administered as needed.
Monitoring And Follow-Up
Continuous monitoring of hemodynamic parameters, renal function, and electrolyte levels is essential for managing hypotension in acute pancreatitis. Frequent reassessment allows for timely adjustments to treatment plans and early detection of complications.
Prognosis And Outcomes
The prognosis for patients with acute pancreatitis and hypotension varies based on the severity of the pancreatitis and the effectiveness of management strategies. Early recognition and prompt intervention are key to improving outcomes. In severe cases, the mortality rate can be high, particularly if complications such as multi-organ failure or sepsis occur.
Preventive Measures
Preventing acute pancreatitis and its complications involves addressing modifiable risk factors:
Gallstone Management: Timely treatment of gallstones through cholecystectomy or endoscopic procedures can prevent recurrent pancreatitis.
Alcohol Moderation: Reducing alcohol intake can significantly lower the risk of acute pancreatitis.
Lipid Control: Managing hypertriglyceridemia through dietary modifications and medications can prevent pancreatitis.
Medication Review: Monitoring and adjusting medications that may increase the risk of pancreatitis.
Conclusion
Acute pancreatitis is a serious condition that can lead to hypotension through various mechanisms, including systemic inflammation, hypovolemia, cardiac dysfunction, sepsis, and electrolyte imbalances.
Prompt recognition, aggressive fluid resuscitation, and comprehensive supportive care are essential components of treatment. By addressing the underlying causes and providing timely interventions, healthcare providers can mitigate the risks associated with hypotension in acute pancreatitis and enhance the prognosis for affected patients.