Heart failure, a condition where the heart cannot pump blood effectively, progresses through various stages. End-stage heart failure, also known as advanced heart failure or stage D heart failure, is the most severe form, where conventional treatments and symptom management strategies become insufficient. Recognizing the symptoms of end-stage heart failure is crucial for managing the condition, improving quality of life, and making informed decisions about care and treatment options.
Overview of End-Stage Heart Failure
End-stage heart failure occurs when the heart’s ability to pump blood is severely compromised. This stage is characterized by frequent hospitalizations, severe symptoms, and a significant impact on daily activities. The progression to end-stage heart failure can result from various underlying conditions, including coronary artery disease, hypertension, cardiomyopathy, and valvular heart disease.
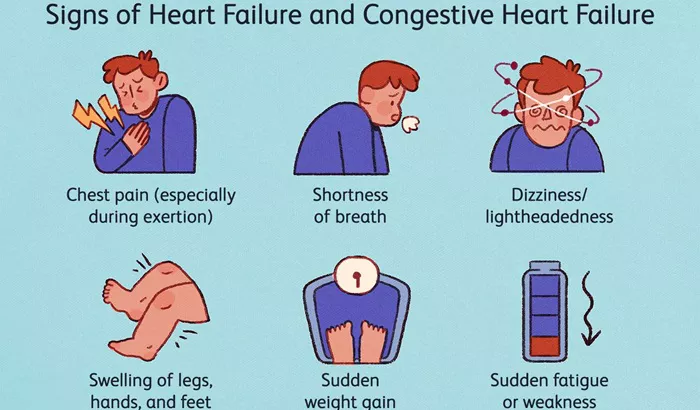
In end-stage heart failure, patients often experience the following symptoms:
Severe Shortness of Breath
One of the hallmark symptoms of end-stage heart failure is severe shortness of breath, also known as dyspnea. This symptom occurs due to fluid accumulation in the lungs (pulmonary congestion) and reduced cardiac output. Patients may experience difficulty breathing even at rest, and activities such as walking or climbing stairs can become extremely challenging. Orthopnea, or shortness of breath while lying flat, is also common, leading many patients to sleep propped up on pillows.
Fatigue And Weakness
The heart’s inability to pump sufficient blood to meet the body’s needs results in decreased oxygen delivery to muscles and tissues, causing significant tiredness and reduced stamina. Simple tasks like dressing, bathing, and eating can become exhausting, severely impacting the patient’s quality of life.
See Also: Is Aortic Valve Stenosis Considered Heart Disease
Persistent Cough And Wheezing
A persistent cough and wheezing are often associated with end-stage heart failure. These symptoms are primarily caused by fluid buildup in the lungs, leading to congestion and irritation of the airways. The cough may produce white or pink, frothy sputum, indicating pulmonary edema, a condition where fluid leaks into the lung air sacs.
Swelling (Edema)
Swelling, or edema, is a common symptom of heart failure, often worsening in the end stages. Fluid retention occurs due to decreased cardiac output and impaired kidney function, leading to swelling in the legs, ankles, feet, and abdomen (ascites).
This swelling can be uncomfortable and may cause the skin to become tight and shiny.
Rapid or Irregular Heartbeat (Palpitations)
Patients with end-stage heart failure often experience palpitations, characterized by a rapid or irregular heartbeat. This occurs due to the heart’s efforts to compensate for its reduced pumping capacity. Arrhythmias, such as atrial fibrillation, are common and can exacerbate other symptoms like fatigue and shortness of breath.
Nausea And Lack of Appetite
Nausea, vomiting, and a lack of appetite are frequent in patients with end-stage heart failure. Reduced blood flow to the gastrointestinal tract and fluid buildup in the abdomen contribute to these symptoms. Additionally, medications used to manage heart failure can cause gastrointestinal side effects, further diminishing appetite and leading to unintentional weight loss and malnutrition.
Mental Confusion And Difficulty Concentrating
Cognitive impairment, including mental confusion and difficulty concentrating, is often seen in end-stage heart failure.
This is due to reduced blood flow to the brain and the effects of chronic illness and medications. Patients may experience memory problems, confusion, and difficulty making decisions, impacting their ability to manage their care effectively.
Decreased Urine Output
A noticeable decrease in urine output can indicate worsening heart failure. This symptom occurs due to reduced blood flow to the kidneys and the body’s efforts to retain fluid to maintain blood pressure. Oliguria (low urine output) or anuria (no urine output) can signify severe kidney dysfunction and require immediate medical attention.
Cold Hands And Feet
Patients with end-stage heart failure often have cold hands and feet. This occurs because the body redirects blood flow to vital organs like the heart and brain, reducing circulation to the extremities. As a result, the skin on the hands and feet may appear pale or bluish (cyanosis).
see also: What Are The Signs of Left Ventricular Failure
Depression And Anxiety
Living with end-stage heart failure can lead to significant emotional distress. Patients often experience depression and anxiety due to the chronic nature of their condition, the impact on their quality of life, and concerns about their prognosis.
Emotional and psychological support is crucial in managing these symptoms and improving overall well-being.
Understanding The Causes of End-Stage Heart Failure
Symptoms
The symptoms of end-stage heart failure are primarily caused by the heart’s inability to pump blood effectively and the resulting systemic effects. Several mechanisms contribute to these symptoms:
Reduced Cardiac Output
In end-stage heart failure, the heart’s pumping capacity is significantly diminished, leading to reduced cardiac output. This decrease in blood flow affects the entire body, resulting in symptoms such as fatigue, weakness, and mental confusion.
Fluid Accumulation
Fluid accumulation in the lungs and other parts of the body is a major cause of symptoms like shortness of breath, persistent cough, and edema. The heart’s reduced pumping ability leads to fluid retention, as the kidneys are unable to excrete excess fluid effectively.
Neurohormonal Activation
The body’s response to heart failure includes the activation of various neurohormonal systems, such as the renin-angiotensin-aldosterone system (RAAS) and the sympathetic nervous system. While initially compensatory, chronic activation of these systems can worsen heart failure symptoms and lead to further cardiac and renal dysfunction.
Arrhythmias
Arrhythmias, or irregular heart rhythms, are common in end-stage heart failure and contribute to symptoms like palpitations, fatigue, and shortness of breath. These arrhythmias can be life-threatening and require careful management.
Reduced Blood Flow to Organs
The heart’s impaired ability to pump blood effectively leads to reduced blood flow to vital organs, including the kidneys, liver, and brain. This results in symptoms such as decreased urine output, nausea, mental confusion, and cognitive impairment.
Managing Symptoms of End-Stage Heart Failure
Managing the symptoms of end-stage heart failure requires a comprehensive and multidisciplinary approach. The primary goals are to alleviate symptoms, improve quality of life, and support the patient’s emotional and psychological well-being.
Key management strategies include:
Medications
Medications play a crucial role in managing end-stage heart failure symptoms. Commonly used medications include:
Diuretics: To reduce fluid buildup and relieve symptoms of pulmonary congestion and edema.
ACE Inhibitors and ARBs: To lower blood pressure, reduce the workload on the heart, and improve symptoms.
Beta-Blockers: To slow the heart rate, reduce arrhythmias, and improve heart function.
Aldosterone Antagonists: To help manage fluid retention and reduce symptoms.
Digoxin: To improve the heart’s pumping ability and control arrhythmias.
Lifestyle Modifications
Lifestyle modifications are essential for managing end-stage heart failure symptoms. These include:
Dietary Changes: Reducing salt intake to help manage fluid retention and following a heart-healthy diet.
Fluid Management: Monitoring and limiting fluid intake to prevent fluid overload.
Physical Activity: Engaging in gentle, supervised physical activity to maintain strength and improve symptoms.
Smoking Cessation and Alcohol Reduction: Avoiding smoking and limiting alcohol intake to reduce the burden on the heart.
Device Therapy
In some cases, device therapy may be recommended to manage end-stage heart failure symptoms. These devices include:
Implantable Cardioverter-Defibrillators (ICDs): To prevent sudden cardiac death by detecting and treating life-threatening arrhythmias.
Cardiac Resynchronization Therapy (CRT): To improve the heart’s pumping efficiency and reduce symptoms in patients with specific types of heart failure.
Palliative Care
Palliative care focuses on providing relief from symptoms and improving the quality of life for patients with serious illnesses like end-stage heart failure. It involves:
Symptom Management: Addressing symptoms such as pain, breathlessness, and fatigue.
Emotional and Psychological Support: Providing counseling and support for patients and their families.
Advance Care Planning: Discussing and documenting the patient’s preferences for end-of-life care and treatment decisions.
Heart Transplant And Ventricular Assist Devices (VADs)
For some patients with end-stage heart failure, a heart transplant or the use of a ventricular assist device (VAD) may be considered. These options are typically reserved for patients who meet specific criteria and have not responded to other treatments.
Conclusion
End-stage heart failure is a severe and complex condition characterized by a range of debilitating symptoms. Recognizing and understanding these symptoms is crucial for effective management and improving the patient’s quality of life. A comprehensive approach, including medications, lifestyle modifications, device therapy, palliative care, and, in some cases, advanced interventions like heart transplants or VADs, is essential for managing this challenging stage of heart failure.
Supporting patients and their families through this difficult time requires a multidisciplinary effort and a focus on compassionate, patient-centered care.