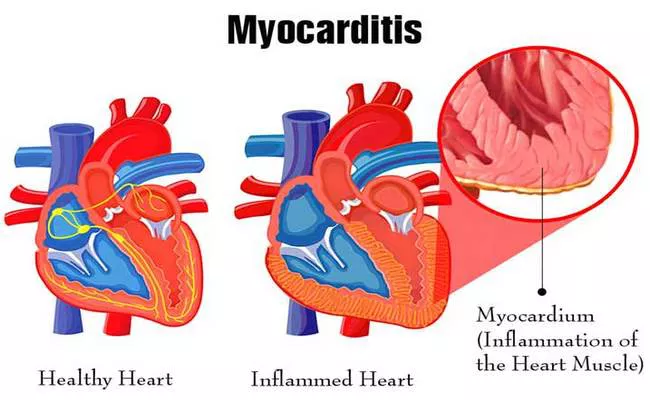
Myocarditis, an inflammatory disease affecting the myocardium—the muscular layer of the heart walls—has emerged as a significant concern in both clinical and public health discourse. Often triggered by viral infections, autoimmune disorders, or environmental toxins, myocarditis presents with varying degrees of severity, from mild symptoms resembling flu to severe cardiac dysfunction leading to heart failure, arrhythmias, or sudden death. A critical question for both patients and healthcare providers is the potential for long-term damage following an episode of myocarditis. This article explores the evidence surrounding the long-term outcomes of myocarditis, factors influencing these outcomes, and the implications for treatment and monitoring.
Pathophysiology And Diagnosis of Myocarditis
Understanding the pathophysiology of myocarditis is essential for grasping how it can lead to long-term cardiac complications. The condition begins with an initial trigger, commonly an infectious agent such as the Coxsackie virus, that directly or indirectly causes inflammation within the myocardium. This inflammatory response disrupts the normal cellular architecture and function of heart tissue, potentially leading to cell death and fibrosis.
Diagnosing myocarditis can be challenging due to its variable presentation. Symptoms range from none at all to severe chest pain, palpitations, or dyspnea. Diagnostic tools include cardiac MRI, which is highly sensitive to changes in the myocardial tissue, electrocardiograms (ECG), which detect electrical abnormalities, and echocardiograms to assess structural and functional changes in the heart. In severe cases, or when the diagnosis is uncertain, an endomyocardial biopsy might be performed to confirm the presence of inflammatory cells in the myocardium.
See Also: How to Strengthen Heart for Running
Short-Term Implications
In the acute phase, myocarditis can impair cardiac function, leading to symptoms such as fatigue, chest pain, and in severe cases, acute heart failure or cardiogenic shock. The immediate treatment focuses on mitigating these symptoms and preventing further damage, often involving medications to manage heart failure, arrhythmias, and in some cases, immunosuppressive therapy to reduce the inflammatory response.
Long-Term Outcomes of Myocarditis
The long-term impact of myocarditis is a topic of ongoing research, and outcomes can vary widely. Recovery without any residual effects is possible, particularly in mild cases. However, some patients may experience persistent or progressive cardiac dysfunction.
1. Cardiac Remodeling and Chronic Heart Failure
One of the most concerning long-term effects of myocarditis is the development of chronic heart failure (CHF) due to cardiac remodeling. Following the inflammatory insult, the myocardium may undergo structural changes, including dilation and fibrosis, which alter the heart’s ability to pump effectively. This remodeling process can be progressive, leading to chronic heart failure with reduced ejection fraction (HFrEF).
2. Arrhythmias and Sudden Cardiac Death
Myocarditis can disrupt the normal electrical pathways within the heart, increasing the risk of arrhythmias. In some cases, these arrhythmias can be life-threatening, such as ventricular tachycardia or ventricular fibrillation, and may lead to sudden cardiac death (SCD). The risk of arrhythmias is particularly elevated in patients who retain significant fibrosis or scarring in the myocardium.
3. Autoimmune and Chronic Inflammatory Responses
In certain individuals, myocarditis can evolve into a chronic autoimmune condition where the immune system continues to attack the heart muscle, causing ongoing inflammation and damage. This condition is more likely if the initial episode of myocarditis triggers an autoimmune response, which may not fully resolve even after the original pathogen has been cleared.
4. Risk of Recurrent Myocarditis
Patients who have experienced one episode of myocarditis may be at increased risk for subsequent episodes, particularly if the initial trigger was an unresolved systemic inflammatory or autoimmune condition. Each episode can potentially lead to greater heart damage.
Factors Influencing Long-Term Outcomes
Several factors can influence the long-term outcomes of myocarditis, including the severity of the initial illness, the patient’s overall health, and the promptness and adequacy of the initial treatment. Genetic predispositions may also play a role in how the body responds to the inflammatory insult and recovers from it.
Preventive Measures And Monitoring
Given the potential for serious long-term consequences, preventive measures are crucial. Patients recovering from myocarditis should be closely monitored for signs of cardiac dysfunction or recurrence of symptoms. Lifestyle modifications, such as adopting a heart-healthy diet, engaging in regular moderate exercise, and avoiding known triggers such as alcohol and illicit drugs, can be beneficial.
Treatment Strategies for Long-Term Management
Long-term management of patients with myocarditis who have sustained heart damage may include medications typically used for heart failure, such as beta-blockers, ACE inhibitors, or ARBs. In cases of severe dysfunction, more advanced therapies like implantable cardioverter-defibrillators (ICDs) or cardiac resynchronization therapy (CRT) may be indicated to prevent sudden death and improve heart function.
Conclusion
While many patients fully recover from myocarditis with no lasting effects, a significant minority can suffer long-term cardiac complications, including chronic heart failure, serious arrhythmias, and recurrent myocarditis. The variability in outcomes highlights the importance of individualized treatment plans and long-term monitoring to manage potential complications effectively. Ongoing research into the mechanisms underlying myocarditis and its long-term effects will likely improve our ability to predict and modify the course of this potentially life-altering condition.